با برنامه Player FM !
Thalamic Stroke: Symptoms, Treatment, and Recovery
Manage episode 426580023 series 2807478
Comprehensive Guide to Thalamic Stroke: Symptoms, Treatment, and Recovery
Introduction
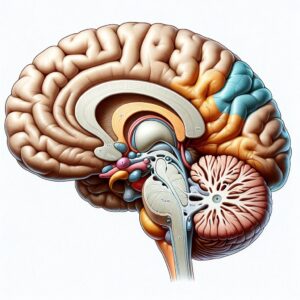
Thalamic stroke is a type of stroke that affects the thalamus, a small but critical structure deep within the brain. The thalamus plays a crucial role in relaying sensory and motor signals to the cerebral cortex and regulating consciousness, sleep, and alertness. Understanding thalamic stroke is essential for patients, caregivers, and healthcare professionals to ensure prompt diagnosis, effective treatment, and optimal recovery.
Understanding Thalamic Stroke
What is a Thalamic Stroke?
A thalamic stroke occurs when the blood supply to the thalamus is interrupted, leading to tissue damage and loss of function in this vital brain region. The interruption can be due to an ischemic stroke, where a blood clot blocks a blood vessel, or a hemorrhagic stroke, where a blood vessel bursts and causes bleeding in the brain.
Symptoms of Thalamic Stroke
The symptoms of a thalamic stroke can vary widely depending on the specific area of the thalamus affected. Common symptoms include:
- Sensory Disturbances: Numbness, tingling, or a burning sensation on one side of the body.
- Motor Impairments: Weakness or paralysis, typically affecting one side of the body (hemiparesis or hemiplegia).
- Pain: Thalamic pain syndrome (Dejerine-Roussy syndrome), characterized by chronic pain on the side of the body opposite the stroke.
- Cognitive and Emotional Changes: Memory problems, confusion, emotional instability, and difficulty with attention and concentration.
- Vision Problems: Partial or complete vision loss, or visual field deficits.
Causes and Risk Factors
The primary cause of thalamic stroke is the obstruction of blood flow to the thalamus. Risk factors include:
- Hypertension: High blood pressure is the most significant risk factor for stroke.
- Diabetes: Increases the risk of blood vessel damage and stroke.
- Atherosclerosis: The build-up of fatty deposits in the arteries can lead to clot formation.
- Heart Disease: Conditions such as atrial fibrillation can cause blood clots that travel to the brain.
- Lifestyle Factors: Smoking, excessive alcohol consumption, obesity, and lack of physical activity.
Diagnosis of Thalamic Stroke
Diagnostic Procedures
Early diagnosis of thalamic stroke is critical for effective treatment. Diagnostic procedures include:
- Physical Examination: Neurological assessment to evaluate sensory, motor, and cognitive functions.
- Imaging Studies:
- CT Scan: Quickly identifies bleeding in the brain.
- MRI: Provides detailed images of brain structures and can detect smaller strokes.
- Blood Tests: Evaluate overall health and identify risk factors such as high cholesterol and diabetes.
- Electrocardiogram (ECG): Detects heart abnormalities that could lead to stroke.
Treatment Options for Thalamic Stroke
Acute Treatment
Immediate treatment aims to restore blood flow and minimize brain damage:
- Thrombolytic Therapy: Clot-busting drugs such as tPA (tissue plasminogen activator) are administered within the first few hours of an ischemic stroke.
- Endovascular Procedures: Mechanical thrombectomy to remove a large clot in cases where thrombolytic therapy is ineffective.
- Surgery: In cases of hemorrhagic stroke, surgery may be necessary to repair damaged blood vessels and relieve pressure on the brain.
Rehabilitation and Recovery
Rehabilitation focuses on restoring function and improving quality of life:
- Physical Therapy: Exercises to improve strength, coordination, and mobility.
- Occupational Therapy: Assistance with daily activities and strategies to adapt to physical limitations.
- Speech Therapy: Helps with communication difficulties and swallowing disorders.
- Pain Management: Medications and therapies to manage chronic pain from thalamic pain syndrome.
- Psychological Support: Counseling and support groups to address emotional and cognitive changes.
Prognosis and Long-term Outlook
The prognosis for thalamic stroke varies based on the severity of the stroke and the promptness of treatment. Many patients experience significant recovery with comprehensive rehabilitation, although some may have lasting impairments. Regular follow-up care and management of risk factors are crucial for preventing recurrent strokes.
Prevention Strategies
Lifestyle Modifications
Adopting a healthy lifestyle can significantly reduce the risk of thalamic stroke:
- Healthy Diet: Rich in fruits, vegetables, whole grains, and lean proteins.
- Regular Exercise: At least 150 minutes of moderate-intensity exercise per week.
- Smoking Cessation: Quitting smoking reduces stroke risk.
- Alcohol Moderation: Limiting alcohol intake to moderate levels.
Medical Management
Managing underlying health conditions is essential for stroke prevention:
- Blood Pressure Control: Regular monitoring and medication adherence.
- Diabetes Management: Keeping blood sugar levels under control.
- Cholesterol Management: Medications and dietary changes to lower cholesterol.
- Anticoagulant Therapy: For patients with atrial fibrillation or other heart conditions.
Conclusion
Thalamic stroke is a serious medical condition that requires prompt diagnosis and treatment. Understanding the symptoms, risk factors, and treatment options can significantly improve outcomes for patients. With comprehensive rehabilitation and lifestyle modifications, many individuals can achieve substantial recovery and improve their quality of life.
Thalamic Stroke Recovery Interview with Jenn Williams
Jenn Williams discusses her thalamic stroke recovery, the risks of the contraceptive pill, and the importance of self-advocacy and resilience.
Instagram
Recrudescence of Deficits After Stroke
Middle People Project
Brain Injury Association Of America
Highlights:
01:52 Introduction
02:48 The Beginning Of Thalamic Stroke Recovery Journey
16:20 Self-advocacy For Medical Care
35:36 Post Thalamic Stroke Recovery And Deficits
43:02 The Middle People Project
51:47 Pain Management And Personal Growth
1:08:50 Insomnia Causes And Solutions
1:17:14 The Hardest Thing About Stroke
1:28:16 Thalamic Stroke Recovery, Grief, And Resilience
Transcript:
Bill Gasiamis 0:00
This episode of the podcast is brought to you by headbed.com.au. Hey everyone. Before we dive into today’s episode, I wanted to share something special. In Episode 305, I interviewed Catherine Randabel, the inventor of HeadBed, a product revolutionizing hair salons, especially for stroke survivors.
Bill Gasiamis 0:21
The HeadBed provides excellent neck and head support during hair washes, reducing strain and promoting better blood flow. For stroke survivors. This means lowering the risk of arterial damage and easing concerns about another stroke. It ensures a safe and enjoyable salon experience and I’m thrilled to support a product that aligns with my mission of stroke prevention and safety.
Bill Gasiamis 0:47
In our interview, Catherine explained how the HeadBeds ergonomic design prevents neck hypertension, a common issue increasing stroke risk. With the HeadBed you can feel confident and comfortable at the salon knowing your health is prioritized.
Bill Gasiamis 1:04
If you’re a stroke survivor or know someone who is HeadBed is a must have for your next salon visit, check out episode 305 for my full interview with Catherine and learn how this product can make a difference. For those in the United States visit head bedusa.com to get yours today and to enjoy peace of mind at the salon.
Bill Gasiamis 1:27
Now I’d also like to mention my book, The Unexpected Way That A Stroke Became The Best Thing That Happened. 10 tools for recovery and personal transformations. If beaches inspiring stories from 10 stroke survivors and offers hope for those on the road to recovery. For more information visit recoveryafterstroke.com/book or search for my name Bill Gasiamis on Amazon.
Introduction – Jenn Williams

Bill Gasiamis 1:52
Now this is episode 309. And my guest today is Jenn Williams, who at the age of 33 experienced a left thalamic ischemic stroke. In this compelling episode, Jenn shares her incredible journey of thalamic stroke recovery, detailing the early symptoms and the misdiagnosis. And the moment her life changed forever.
Bill Gasiamis 2:14
Jenn also discusses the emotional and physical challenges of recovery, the risks associated with taking the contraceptive pill, and the importance of self advocacy. She highlights the impact of gratitude, community support, and how she has turned her experience into a mission to help others through her work with the Brain Injury Association and The Middle People Project. Jenn Williams, welcome to the podcast.
Jenn Williams 2:41
Thanks for having me.
Bill Gasiamis 2:43
Thank you for being here. Tell me a little bit about what happened to you.
The Beginning Of Thalamic Stroke Recovery Journey
Jenn Williams 2:48
So it was 2016. And I was working as an insurance agent in a busy office and my wrist and my hands on my right side kind of got that feeling like it was falling asleep while I was at work. And I kept trying to shake it out like you do when your arm falls asleep or something and it wasn’t working. I made a very poor joke now looking back to my coworker and said if I die, this is how this started.
Jenn Williams 3:19
Yep. So the next day, I had that same tingling in my foot on the same side and half of my face. So I got into see my primary care. And she said, you know, we’ll run some blood tests, it could be a mineral deficiency, you know, all this other stuff. There was some miscommunication on what the tests were supposed to be.
Jenn Williams 3:45
So I went in and out a few times. I believe that was a Tuesday when that all started. And then by Friday of that week, the tinkling was my whole right side. So I had a follow up the following Thursday, and my husband was meeting me at the appointment, he was taking some time off from work, because we didn’t know what’s going on and I wanted some support.
Jenn Williams 4:08
And I drove from my house to the appointment. And by the time I got there, I didn’t feel good at all. I don’t feel right, my stomach is turning, I’m dizzy. I went to go get out of a car and I fell onto the hood of the car and my husband was like what is happening right now? We went into the appointment and she said, we’ll order some tests. You know, we’ll give you a call and let you know.
Jenn Williams 4:35
And during this appointment, my husband called his mother to come get my car because I said I don’t feel safe driving. There’s something going on. And in the 10 minute ride that it took to go from the doctor’s office to my house I was paralyzed. And I don’t know about you but I was raised to believe you know the doctor is the end all be all.
Jenn Williams 4:58
That’s what they do. That’s what they you know, you believe what they say. So I looked at my mother in law, and I said, It’s okay, I’ll just wait for the doctor. And she screamed and said, This is not okay. And she took me to the ER. And they found that I had had a left thalamic stroke, ischemic so clot.
Jenn Williams 5:22
And I was in ICU for about three days, they wanted me to go to inpatient rehab. But my family and friends were like, we’re not doing that we’re not going to do inpatient, we’ll just help you at home. So I was fortunate enough to go home after leaving the ICU. And I had a lot of support for those three weeks.
Jenn Williams 5:41
But as many brain injury survivors know, there’s a lot of tests and things that proceed after that. And there was no real issues that they could determine no clotting disorder, no high blood pressure, no diabetes, nothing like that.
Jenn Williams 6:00
So the general idea is that it was caused by medications, I was taking contraceptives and migraine medications, which both have those dangers, and family history, there is some family history. So definitely not what I expected in my life, at age 33. At the time. But it’s been a really educational incredible experience.
Bill Gasiamis 6:26
Yeah, you know, you’re not the first person I’ve interviewed who was taking a contraceptive. There’s, I dare say there’s at least another two or three and younger as well, kind of in their 20s. And what’s interesting is when I asked them did you know about that risk? They all said no.
Bill Gasiamis 6:54
And even if they did, no, I’m not sure that it would have changed anything if they were told, by the way, this medication has this risk, but I don’t know if it would have changed anything. Because I know sometimes contraceptive pill is taken for non contraceptive reasons. Yeah, so were you aware that it was a risk that came with taking the contraceptive pill?
Jenn Williams 7:24
Yes, I didn’t know I started when I was in high school. And I didn’t realize at that point, but then as I got into adulthood, I started reading those packets that they give you when you leave the pharmacy. And I honestly, I think it was one of those things where I said that’s for old people. That doesn’t happen to young people.
Jenn Williams 7:43
That’s not going to happen to me. And, you know, I was on contraceptives for 25 years. And I just assumed it wasn’t going to happen to me. Yeah, but I can I kind of go on a tangent. Is that okay? One of my biggest frustrations, this whole process has been the realization that a significant percentage of the population has clotting disorders.
Jenn Williams 8:13
And we just prescribe medications, especially contraceptives, we just prescribe them to young girls, and we don’t check for those things. And that makes me so scared for our general population, but scared for like my nieces. That I mean, that’s a horrible. I mean, yes, I’m grateful for it in so many ways, but it is a really horrible experience. And I don’t wish that on anyone. And I don’t understand why we don’t check people for things like that. Before we prescribe medications.
Bill Gasiamis 8:44
I love that because that’s the biggest issue is these know, what’s the word? There’s no kind of investigative work done. Yeah. Before somebody says you should take this. I mean, I know even my father in law, who’s in his 80s. He’s on like, 55,000 medications. But when even though he’s on so many, nobody still does the whole, I wonder if this is going to be appropriate for you to take because that might interact with that and that might do that and that.
Bill Gasiamis 9:18
And my wife, she’s a bit of a how can I describe her? She’s a bit of a like a detailed freak, like she does details about things that most people would just roll their eyes out, right? It’s just her nature. She’s very thorough, and all that type of thing. And if it wasn’t for her dad would be taking medication that instead of lowering his blood pressure is making it worse or you know, they’re giving him stuff that works with the blood pressure medication to lower even further.
Bill Gasiamis 9:57
And she’s the one doing the research and he’s been in the system forever. And and it’s really scary to be a family member and to put all your trust in the medical system and not question it. I think that’s kind of a little bit of putting your head in the sand kind of scenario. And I was trained like that as well, when there was something wrong. My parents took me to the doctor, and whatever the doctor said, what we did, and thankfully, all worked out well. But if I took that approach, when I went to hospital for my first bleed.
Intro 10:35
If you’ve had a stroke, and you’re in recovery, you’ll know what a scary and confusing time it can be, you’re likely to have a lot of questions going through your mind, like, how long will it take to recover? Will I actually recover? What things should I avoid? In case I make matters worse, doctors will explain things.
Intro 10:54
But obviously, you’ve never had a stroke before, you probably don’t know what questions to ask. If this is you, you may be missing out on doing things that could help speed up your recovery. If you’re finding yourself in that situation, stop worrying, and head to recoveryafterstroke.com where you can download a guide that will help you it’s called a seven questions to ask your doctor about your stroke.
Intro 11:19
These seven questions are the ones Bill wished he’d asked when he was recovering from a stroke, they’ll not only help you better understand your condition, they’ll help you take a more active role in your recovery, head to the website. Now, recoveryafterstroke.com and download the guide. It’s free.
Bill Gasiamis 11:38
Well, nothing my first paid for my second bleed, then I would have been completely dissatisfied with the level of care that I was receiving. And 37 When my life’s on the line, I’m like, Well, I don’t think I’m going to cop this, you guys aren’t going to be that way while I’m around. And I’m going to do something about it.
Bill Gasiamis 11:57
And then I took responsibility for those things. Luckily, I was able to I was cognitively well enough just to be able to take responsibility for that stuff and to handle some of that stuff off to my wife. And, and we got through it. What bothers me about women who have taken them the the contraceptive pill, and they’ve been on my podcast, is that one of them, ask them? Did the doctors say it was the pill that did it. They do the hall while it may have been the pill that did it.
Jenn Williams 12:33
Yeah, they won’t cop to that.
Bill Gasiamis 12:36
Yeah, no one commits to it. It doesn’t say it on the box for no reason it says it on the box for a reason. And when you’re perfectly healthy, you don’t have any history for any of those conditions that cause blood clotting disorders. And you’re young, and you have a stroke, and you’re on that there should be a logical conclusion.
Bill Gasiamis 13:02
And this shouldn’t be this. We’re just going to wipe our hands from that, but I think that is the pharmaceutical industry, right? That is that whole, just give them this stuff. And you know, 99.9% out of the time, it won’t cause any harm, and it won’t cause any problems. And if it does, we’ll just deny it anyway, it will say it could have been something else.
Jenn Williams 13:25
Right? So they classify my stroke as cryptogenic. Because they’re not gonna say that it was officially the contraceptive. So they say that there’s no known cause. Well, if I don’t have any of the other risk factors, I don’t smoke, I take very good care of my body.
Jenn Williams 13:44
All of my numbers are good. Then what does that leave? But it’s like they’re too scared to say that. Which is really unfortunate because it leaves so much unanswered for people that are like myself, like you that are looking for answers.
Bill Gasiamis 14:02
And you’re looking to maintain your health as much as possible. Now that you’ve had a stroke, you want to make sure you don’t have another one. Did anyone say you should stop taking the contraceptive pill?
Jenn Williams 14:16
Oh, yeah, that was the first thing that the doctor said to me. Well, thank goodness.
Bill Gasiamis 14:20
Oh my gosh. So it probably wasn’t the contraceptive pill but stop taking it anyway.
Jenn Williams 14:25
Oh, yeah. Then the neurologist in the ER came to me and said you will never take contraceptives again. That was in the ER before I was even admitted to the ICU. Yeah.
Bill Gasiamis 14:40
I many years ago was coaching a lady who wasn’t on the contraceptive pill but she was on other medications. stuff again that she started in her teenage years for some conditions right for a particular condition.
Bill Gasiamis 14:54
And by the time I spoke to her, she might have been 2530 years into taking that particular medication. And the very first question I asked her was, is it still necessary for you to take that medical medication? Has that issue resolved? And she looked at me dumbfounded. She goes, I don’t know. I’ve never asked anybody. I just go and get the refill every, every however often, and I just take it again.
Jenn Williams 15:23
I just keep taking the medication.
Bill Gasiamis 15:26
And I was like, okay, cool. So the next time we spoke, she had spoken to her general practitioner, and they had begun the process to investigate her condition and her situation. And to determine whether or not it was a good opportunity to start removing herself from this particular medication stopped taking this medication.
Bill Gasiamis 15:50
And no one had followed up with her in all those years, and no one had said, How’s this going? How’s that going? In Australia, you have to go back and get a script, from your doctor, every so often, they’ll give you certain refills, and the pharmacist where you pick up the medication all day, every day, your entire life knows you by name by now, nobody kind of goes, what are you still don’t take in this, how are you going? Are you better? Have you recovered?
Jenn Williams – Self-advocacy For Medical Care

Jenn Williams 16:20
And I think I think that too, comes down to the piece of self advocacy, advocating understanding your body but also advocating for your body. And I’ve been very clear with my doctors, I don’t want to take on unnecessary things. How long have I been on this? Can I get off of this? And they know that that’s my stance. So I think being very clear and direct in that way can be really helpful. But like you said, a lot of people just don’t even think about it. They just, I gotta go get my meds and they take their meds and they go about their day, not thinking that they’re putting chemicals in their body and causing potential damage.
Bill Gasiamis 16:58
And disclaimer, neither Jen or I are saying, stop taking your medication. No, one’s saying that.
Jenn Williams 17:06
Good call Correct. No, one’s saying that or saying talk to your doctor.
Bill Gasiamis 17:11
Correct. And we are also saying that some medications are very necessary, and you have to keep taking them. And you must not be slug are taking them because they’re probably keeping your well and healthy. So there’s both sides of the spectrum. And we’re encouraging people just to know, just, yeah, where they’re at.
Jenn Williams 17:38
Just to ask, it’s and so I’m from Maine in the United States, and we’re the most northern state on the East Coast. And I do self advocacy training with support groups with a colleague from New Hampshire. And one of the things we tell people is, it’s your body, you have the right to ask questions about your body and about your care. That’s so important. It’s okay to ask a question. And so many people are too scared. It is okay to ask a question about your body. It’s yours.
Bill Gasiamis 18:13
I agree. I think maybe do you think maybe the recent pandemic challenges with medications might have thrown a bit of a spanner in the works, the way that they were suggested that they were taken, might have thrown a spanner in the works to comply.
Jenn Williams 18:34
In a way, I do think that there are some people that are and this is not a dig at anybody, but that there are more apt to comply than others. And for me, once again, I needed to do what was right for my body. And for me, I felt like we didn’t know enough yet. And I was not comfortable taking any vaccinations or anything like that. And I had a lot of people that were really mad at me, including my mother for making that decision for myself. And now looking back, I made the right decision. I don’t knock anybody for doing that. It’s just your own personal decision.
Bill Gasiamis 19:14
Same and on that point of the thing that you said I think which is the best you didn’t know enough. And you not only did you not know enough about that. But this is the point that’s the exact point. Most people don’t know enough about taking the contraceptive pill. Most people don’t know enough taking x y z and that’s the thing it’s that we don’t know enough, we haven’t asked enough, we haven’t learned enough, we don’t understand the ramifications, the complications, we don’t understand that.
Bill Gasiamis 19:43
I think we should understand it. Especially if the ramifications of not taking something as well and negative so blood pressure lowering medication, blood sugar lowering medication like if we are not doing other things As to support our blood pressure and our blood sugar. And we need medication.
Bill Gasiamis 20:05
We need to know the ramifications of the other side of the spectrum. What happens if you don’t like high blood pressure medication? stops people from having hemorrhagic strokes? And ischemic strokes? So we need to know more. And thank you for going on that tangent. That was a good one.
Jenn Williams 20:26
I think it comes with brain injury honestly.
Bill Gasiamis 20:30
It’s very relevant. Why don’t want to do that. I want to go back to before we went on that tangent, and I want to ask you about how did you end up leaving hospital with your family with you in the care of your family? And what kind of a decision was that that they made that they were going to take the responsibility for helping you get through this on? Like, how does that happen?
Jenn Williams 20:56
I mean, partly, I think it’s just that I’m just wildly independent, and so is my mother. And my mother is not going to accept me being coddled, I guess. It’s just not how I was raised. I was raised to be, you know, very independent and forthright. So I, they came in and they said, we really want you to go to inpatient rehab, it would be three to six weeks, you would have your daily PT, OT, those kinds of things.
Jenn Williams 21:31
And my mother was, no, because she’s seen family members go to inpatient rehab. And we said, okay, so what would outpatient look like, you’d be going to the outpatient facility three days a week, you would have your PT or OT, I did have a speech evaluation, which they just said, You’ll get better. And I didn’t have to go for speech therapy. But they really they kind of explained that the outpatient therapy was actually more intensive than inpatient therapy, because they have more tools in their outpatient centers than they do in inpatient.
Jenn Williams 22:11
So that was the other deciding factor was that when I first went to the neurologist, after my stroke, I didn’t understand. And I said, how long is this going to take? Like three months, I don’t have time for this. And now looking back, that outpatient decision was the right decision, because that was my attitude, going into it from the beginning, is I’m going to get better. I’m going to walk again and write again, and all of those other things, it’s not negotiable.
Jenn Williams 22:41
So how do I do that? That’s the most efficient way possible, which was outpatient. And I had an amazing experience with my outpatient rehab. And during the days, when I had appointments, my mother would come and take me. And then on the days where I didn’t have appointments, and my husband was at work, I had friends and family that would come and spend the day with me, because I was a fall risk.
Jenn Williams 23:04
So make sure that I, you know, could go to the bathroom. And that kind of thing. I wasn’t allowed to cook, because I couldn’t tell temperature in my hand. And of course, there’s all cognitive pieces to that as well. So I had friends and family that would come over and make me lunch and that kind of thing. And then in the evenings on the weekends, my husband was the caretaker.
Bill Gasiamis 23:28
That’s very cool. I get it now. That’s a great move. I thought that they took on your care. And I had no tools or sir or capabilities or skills to do any of that stuff. And I was fascinated to hear that story. But I think what you did was awesome, because I was in inpatient rehab for about a month. And I was I was like you I was maybe it wasn’t how long is this going to take but it was I’m going to put as much time and effort in as I can while I’m here to get a result. So I’d go home sooner.
Bill Gasiamis 24:05
And instead of being in for the two months that they had booked me in for was in for a month. And then I went to outpatient rehab and I had a similar kind of support structure where family would take me to and from. And my level of cooking was just low level of, you know, prepping a sandwich or something simple that didn’t require knives and standing for too long and all that type of thing.
Bill Gasiamis 24:36
And then family was bringing over food and then my wife when she wasn’t at work she was helping out and doing her her bit. So it was very similar. And I remember going to outpatient rehab, but I felt like it was a bit of a waste of time. I felt like I had done the majority of the recovery I got great results at in inpatient rehab. And then outpatient rehab, I ended up getting to the point where I said to the guys, I think I think I’m done with you guys, you’ve done a great job, and I’m gonna take the responsibility to improve my walking even more.
Bill Gasiamis 25:20
On my own, I’m going to do that at home, and I’m going to get better at home. But thanks for everything that you did. And one of the reasons I did that was because I was bothered. I had three appointments a week. And after about, say, nine months of best six months of outpatient rehab, that meant that I had to spend, and always around the middle of the day or something like that I had to spend half of the day, going to the appointment, doing the therapy, and then leaving the appointment and coming home.
Jenn Williams 25:59
And recovering from those appointments takes a lot out of you as well.
Bill Gasiamis 26:04
So it’s about three or four hours of the day that are gone. So I couldn’t be productive in other things. So it was kind of weighing up the all the pros and cons and then going, okay, the pros are that I’m really well, well enough to go home. And then I can definitely do more recovery on my own and save three or four hours, three days a week.
Jenn Williams 26:34
And I asked my physical therapist, I said, you know, how like, would you classify this injury as, because I call them a brain injury? would you classify this is like, mild, it doesn’t feel mild, because I’m learning to walk again, and learning to write again. And she said, I would call it moderate. And I said, I’m just trying to figure out if my recovery is because I’m younger, and I have more gray matter and I more easily leave covering, or if it’s because of like the type of stroke. And she said, Honestly, it’s because you show up.
Jenn Williams 27:12
And I said, What do you mean I show up? Of course, I show up. And she said the amount of people that don’t show up to their appointments is shocking. And when you miss an appointment, you miss a step in your recovery, just like you show up, you do the exercises, even if they scare you and make you uncomfortable, you still try them. And you you try and you show up and you do the work. And that’s what has made a difference in your recovery.
Bill Gasiamis 27:38
I would tend to agree with that. And even if it’s hard, you do it, even if it’s hard, and you do it even if you’re fatigued later. And even if you have to recover for half a day or a day.
Jenn Williams 27:51
And I cried in PT all the time. It’s just part of the process.
Bill Gasiamis 27:57
Yeah, you have to kind of push yourself, you’ve got to get beyond your limits. You got to find where your limits are. You’ve got to do everything. And it’s got to be you’ve got to be brave to just go places you’ve never been before emotionally, mentally, physically. Because you do get results, you get something back. Now, it might not be the same thing, everyone might not get the same thing back.
Bill Gasiamis 28:22
But you always get rewarded for putting in more effort when your effort is going towards trying to make you walk better use your hand better, balanced better, you’ll always get a reward by putting in more effort, especially when it’s supervised and you’re safe. And you’re in a good place. Why I like to think that people who are listening to this podcast or other podcasts that are related to health and wellness and recovery.
Bill Gasiamis 28:53
And overcoming challenges, and all that kind of stuff are always going to be better off than the people that are not looking for podcasts, to listen to, to learn from books, who are not asking to be on a podcast. It’s like, I don’t know what your condition is. I don’t know how bad you are. But if you’re on my podcast, or another person’s podcast, who talks about recovery and overcoming stuff, and how you’re beating the odds and all that sort of thing, you are likely to get a good outcome, you are likely to have an amazing life in 10 years from now.
Bill Gasiamis 29:27
And the people who aren’t I’m not saying if you’re listening, that’s not enough. No, that is enough. All I’m saying the people who aren’t considering any of that stuff, and are just feeling sorry for themselves. They are going backwards, they’re not going to achieve much.
Jenn Williams 29:46
And that’s another thing that I share in, you know, the trainings that I do is that part of my because people ask me, you know, how did you have such a great recovery? And one of the things I say is that I refuse to be a victim I’m not going to let this one medical trauma, destroy the rest of my life. I’m not going to sit back and say what was me and just be depressed for however many years I have left, too young for that that’s not acceptable to me. So I’m not going to be a victim. I’m not going to sit there and let life pass me by. And I think that that mindset makes a huge difference in recovery.
Bill Gasiamis 30:28
This this is saying that I’m gonna ruin right. And I’m gonna not say it right, for sure. It goes something like you fail 100% of the times you don’t try. So I’ve taken that to heart. It’s like, every time you’re afraid of something failing, because you tried it, and you weren’t good enough at it at the beginning. That’s not a failure. That’s a win every time you thought, I’m not going to do that in case I fail.
Jenn Williams 31:02
And you’re learning, you learn every time you fail at something.
Bill Gasiamis 31:08
So tell me a little bit about your background. What did you do for work? What were you doing to occupy your time before you had the stroke?
Jenn Williams 31:19
I was in banking for about 10 years. So I worked in commercial lending, I worked in the branch doing teller work, and I became a licensed insurance agent. A couple of months before my stroke, yeah. See, we I got my job in October of 2015. My husband and I bought a new house in January of 2016. I became a licensed insurance agent in May of 2016. And I had my stroke in August.
Jenn Williams 32:02
So I continued to try and go back to work. That was not not conducive. But I was I’m also a 31 consultant. So it’s direct sales. And there’s like bags and totes, and that kind of thing. So and I was a leader in that company. So I was working 40 or 50 hours a week as an insurance agent, about 15 or 20 hours a week at that job. And I was going to CrossFit three days a week.
Jenn Williams 32:31
I was actually continuing to try and go to CrossFit when my hand was tingling. And I was adjusting movements over that 10 days, because I couldn’t grasp correctly. But I mean, not that I don’t now but I had a very full life. It’s just a very different full life. Now I, you know, spent a lot of time with my family and made sure that I had a lot of fun things scheduled and to concerts and all that other stuff. I tried going to a concert, I think two or three years after my stroke, that was not a good idea.
Jenn Williams 33:08
I’m better now. But the sensory overload that Oh, my goodness. And that has been one of my biggest issues is overstimulation and sensory overload. Which I’m sure as you can understand, and I’m sure other people have said this on your podcast is that when people can’t see it, they don’t know it’s there. They don’t understand.
Jenn Williams 33:28
So they just say, Oh, you look great. You’re fine. But constitutively No. So I tried going to a concert, and it was not a good idea. I’m almost eight years post injury and I can do those now. But I’ve had to definitely adapt my life, it’s not what it used to be. It’s different. Does that answer your question?
Bill Gasiamis 33:52
It does. I wanted to get a sense of like, how you were and how you hang out now what you do now. I was the same. You know, work was no problem. I was 37 It was everything was happening fine. Tried to go back to the football which was the thing and people would invite me to go to the football I said I think I want to avoid that I don’t want to go there’s too much noise and yelling and cheering and bright lights for a night game and all that kind of stuff. And it was really difficult to be there.
Bill Gasiamis 34:24
Tried to go to a couple of venues where family would have a party or something like that or get together and then that would be an early night a lot of the times you’d be I think I’ve had enough at around 930 or 10 o’clock and it’s this go home and then I did go to an AC DC concert with my sons and here in Melbourne and I went with ear protection so that it can dial the right sound a little bit and I could still be there because of my Favorite band.
Bill Gasiamis 34:57
And then I still will avoid loud rooms, if I can noises, TVs and all that kind of stuff. Everything’s always on, you know, as low as possible. And even these lights that I have next to me and, and in front of me on the podcast where I where I record, even they bugged me. They’re on for an hour. And they bugged me. But like, yeah, you need, you need some lighting, so I can put up with it for now. So it’s okay. So what deficits do you have now? How does the body feel now?
Post Thalamic Stroke Recovery And Deficits
Jenn Williams 35:36
I’m mean, overall, I’ve had a really good recovery, I still have my struggles. But I’m really grateful for the recovery I’ve had, I still have some balance issues. I started going to yoga and bar. I don’t know if you know what Barr is. It’s like a combination of like ballet, yoga and strength training. So it really focuses on those little muscles, which I realized is what I needed to focus on to help my balance. So that’s been helping very slowly, but it’s a very, very slow process. So balance is still an issue, and insomnia.
Jenn Williams 36:18
I have terrible insomnia. It’s really bad. I’ve been working with a naturopath to try and get that fixed because I was not getting answers in the standard medical world. And then cognitive, really, that overstimulation? I call it delayed memory, like I will remember things a couple of days later, which I had a neuro psych evaluation. And they said that that’s actually stroke onset ADHD, I didn’t know that was a thing. So it can’t be treated with medication because it’s due to brain damage. So I just kind of have to navigate as best that I can with all of that.
Bill Gasiamis 37:04
And stroke onset ADHD makes you remember things two days down the track.
Jenn Williams 37:11
So it’s because if I’m not in a focused environment, like right now, if you and I are talking, and you know, my husband comes in and says, you know, hey, can you do this when you’re done? I won’t remember that. If he says, Hey, I need your attention. And they says, Can you do this? Yes, I can. But it’s because of that distraction, that ADHD that I had my testing done, and they said, my storage and recall is fine. It’s just that there’s this delay in me finding the information that I have stored in my brain.
Jenn Williams 37:44
And it’s because of distraction. So that’s been an adjustment, I’m trying to use post it notes and alarms on my phone, and calendars. And I have the calendar on my phone, and I have a paper calendar. And then I have a family calendar, and I have all of those things to make sure that things don’t fall through the cracks, cracks, they still do sometimes. But that’s been an adjustment, as well.
Jenn Williams 38:12
And then that overstimulation piece like I mentioned, the hardest thing for me has been the grocery store and driving. Those are very complex tasks for the brain, and you don’t realize it until your brain is misfiring essentially. So I’ve worked really hard to get to the point where I can do those things. I don’t know if you guys have this in Australia, but there’s a company in the United States that does music therapy for cognitive health.
Jenn Williams 38:43
And I use them which made a huge difference. And I went from not being able to drive for more than maybe 15 minutes to driving an hour, hour and a half. And like going having lunch with my friend and driving back in an hour. So that made a really significant difference in my recovery. But when I’m tired that all flares back up.
Bill Gasiamis 39:06
And then the brakes get put on I know that I know that when I’m tired thing the wall comes up from out of nowhere.
Jenn Williams 39:15
That’s a great description a great analogy “The Wall” it’s exactly what it is.
Bill Gasiamis 39:20
That’s what it is. And it’s like I’m here again. All right. Okay, I’ll stop I’ll sit down and won’t do anything now for the next however many hours and for me the wall’s getting shorter and shorter. But it still pops up it still kind of says you’ve done too much. You haven’t rested enough you didn’t have a good night’s sleep. Time to sit down and do nothing. And that’s it and everything just sort of shuts down like you say like in the movies. You know when a button is switched off on the robot and everything just goes.
Jenn Williams 39:56
Powering down.
Bill Gasiamis 40:02
That’s exactly it. So, man, I was gonna ask you a question about something you just said about your Oh, yeah. Music therapy. So what’s that based around? Is it based a certain frequency range that you listen to? How does that work because I have used, and we do have people who offer music therapy.
Bill Gasiamis 40:29
I’ve never gone to a music therapy session, but I have listened to certain meditations that are at certain frequencies, to get certain waves, beta waves, theta waves, all that kind of stuff going, depending on what you want to achieve. So tell me about what you did.
Jenn Williams 40:47
So this is what I experienced is different than that. But I do use those meditations, like you mentioned, especially delta waves for sleep, so I use those. But this music therapy was to help me with my divided attention, the stroke onset ADHD. And basically, what the therapist would do is she would have a guitar.
Jenn Williams 41:08
And then she would have a drum playing on her computer. And she would say, random letters, and I had to raise my hand whenever I heard an H, but only if the drums were playing. So I had to listen to her guitar, listen to the letter, listen to the drums, and then make a decision and acknowledge it physically with my hand.
Jenn Williams 41:32
Our pool is very complex, but their intake, you know, they do an intake and you know, our exam, just like any other provider, my intake, I was at, like 67% accuracy. And when I left, I was over 90%. So there’s proof in those that that made a difference, for me a significant difference. So there was a lot of different things like that, or she would tell me, she would play notes.
Jenn Williams 42:02
And I had to tell her, basically, whether they were the notes were going up or down from the previous one. So I have to listen and kind of process the two different tones. Was that first tone lower? Or is the second tone lower? So that required some additional divided attention as well. So it was really it was really interesting.
Bill Gasiamis 42:27
Did you also learn you weren’t tone deaf?
Jenn Williams 42:30
Yeah, I used to play music and in school and like high school, so I know I’m not tone deaf. Not completely anyways.
Bill Gasiamis 42:44
Good. I’m glad you got that.
Jenn Williams 42:46
I did I like it.
Bill Gasiamis 42:50
That’s cool. He’s mentioned earlier a little bit about advocacy work that you do about that? What do you do? Who do you hang out with? What? What spaces do you do that in?
Jenn Williams – The Middle People Project
Jenn Williams 43:02
So I’ve done some speaking at some support groups, I’ve done some speaking to college classes for future like speech language pathologists, to kind of talk about brain injury and how they can actually make a difference in brain injury or recovery. I can I plug I don’t want to like plug a business or anything.
Jenn Williams 43:30
But I want to tell you about this project. So I told you I was teaching self advocacy with a colleague from New Hampshire. So I also am on the advisory board for the Brain Injury Association of America, Maine chapter. So they look for survivor’s input. And I also did some administrative support for our legislative council that deals with brain injury law.
Jenn Williams 43:58
And in all of those meetings, I have said, what about the people in the middle? Because they talk a lot about these, you know, government waivers and Medicare and you know, how many spots we have and who’s getting services and all this other stuff? Well, those are very small numbers.
Jenn Williams 44:18
So what about the people in the middle? What about the people like me, that didn’t go to inpatient rehab, I went home, I did outpatient for a year. And I’ve been trying to figure it out on my own for eight years now. I stuffed the primary group that I see at support groups these people that aren’t eligible for certain services, either because they’re “not disabled enough”, which I’ve been told, or they don’t meet qualifications financially.
Jenn Williams 44:50
So they’re just left to not much for resources. So I shared this idea over and over again, wasn’t really welfare saved. And then I shared it with my colleague from New Hampshire, John, and he shared it with his colleague, David. And David took it and ran with it. He was like, this is an amazing idea. There’s millions of middle people if you actually break down the numbers.
Jenn Williams 45:15
So the three of us have started The Middle People Project. So we’re trying to create a hub of resources for people that feel like they’re in the middle. They don’t qualify for services, but they feel like they still need help. And they’re not as fully recovered as they’d like to be. I don’t think anyone ever fully recovers. So I don’t like to use that term.
Jenn Williams 45:36
So we’re trying to offer self management strategies, and eventually do you know, a blog and helpful resources, that kind of thing, because there’s so many people that just need a little extra support, and they don’t know where to go. So that’s another kind of passion project that I’ve been working on in the brain injury world, I have all sorts of ideas. So we’ll see where, you know, next year, I could be on a totally different project. I don’t know.
Bill Gasiamis 46:07
Yeah, well, if you’re ADHD brain has anything to do with it, you definitely will be.
Jenn Williams 46:12
Oh, it does. That’s why I have notebooks everywhere.
Bill Gasiamis 46:19
Yeah, that’s really cool. So I was one of those people stuck in the middle, I received some health care, and some rehabilitation, got a really good result was happy, didn’t feel like the job was done, and then wanted to do more. And then continuing to do more, I consider myself fully recovered, but not from the damage that was done, the damage is there, and my deficits are there. But if I call myself fully recovered, it’s probably from the emotional side of that. And the mental side of it. Although I did my book launch about a week and a half ago.
Jenn Williams 47:00
Congratulations.
Bill Gasiamis 47:02
Thank you, thank you. I was in tears. So often in my presentation in my speech, and I had to start making jokes about it. And during the presentation, it was so there was so much of it. And I didn’t realize I was going to have such an outpouring of emotions in that way that it was going to be so evident. And I had to catch myself a few times. But the good thing about being emotional in front of people is, as soon as you cry, you’ve got them hooked. So it didn’t matter, every time I thought I was losing them, I just chucked a few tears out there and just bring them back again.
Jenn Williams 47:02
Yeah. So I applied to speak, to share my survivor story at the main brain injury conference this fall. And because of all my work, I know quite a few people at the Brain Injury Association, and one is my friend Sarah. And I would say it was like two weeks after I applied. I had a really long day at my job that I have now, which is working at a property management company. And I overdid it. And I realized that I was at the office and I couldn’t drive home.
Jenn Williams 48:20
So I ended up laying on the floor for like a half hour until I felt safe to drive home. And I’m on my way home, just sobbing. And I call her and I’m like, who am I need to talk about recovery and mindset, if I am sobbing in my car, eight years later, and I overdid it. And she’s like, that’s why that’s literally why because that’s relatable because survivors deal with that every day. And I just had this moment of like, I don’t have this under control at all. I thought I did, but I don’t.
Bill Gasiamis 49:03
Exactly. I’m 12 years out and here I am speaking in front of a whole bunch of people who came to see me talk about a book, you know, and I think that just goes to show that that’s, you know, that’s just human that’s just being human that’s that’s all that is, not anything else. And it’s good to be able to share your express your emotions, to have the understanding as well, that I need to lie down, I can’t drive and rest.
Bill Gasiamis 49:31
I often would find myself jiving many years after the brain surgery and kind of get the whole nods happening you know, oh my gosh, don’t think I’m I’m fading. All over Find a quiet spot under a tree had just sleep. Sit down, say for 2030 minutes as long as I needed. And then I would start the car and go again.
Bill Gasiamis 49:59
And it was necessary, without it, I definitely would not have made it home safely. And it was simply because of that overwhelm of perhaps the distance I traveled, the amount of time I was concentrating cars going by whether it was raining, or whether it was sunny, everything impacted, the way that I would experience that drive and everyday was different.
Jenn Williams 50:27
Driving is a very complex thing for the brain, there’s a lot of input that’s happening, you’re looking at the road in front of you, you’re looking at the road to the left or the right, depending on what country you’re in, you’re looking at the other lanes watching the traffic, you’re looking on the side of the road for any potential hazards, you’re looking in your rear view and your side mirrors.
Jenn Williams 50:48
And for me, the biggest issue that I was dealing with was the shadows from the trees, at certain times of day, they would create like a strobe effect. So it felt like a strobe light while I was trying to focus on all of those things. And similarly, like you said, if it’s raining, raining with the windshield wipers, it would feel like a strobe going in front of my eyes. So it just you don’t realize how complex it is until your brain is trying to basically learn it all over again.
Bill Gasiamis 51:20
Yeah, that’s that’s a legitimate reason to feel like you need to lie down and restaurant you have to it’s yes, it’s necessary. 100%. And I’m like you like it does make me doubt my qualification of being a podcaster promoting all this stuff. And, you know, being an advocate and all that something kind of does make me question my qualification.
Pain Management And Personal Growth
Bill Gasiamis 51:47
And makes me do silly things like, it makes me have like, imposter syndrome every once in a while still. And all that type of stuff. It’s crazy. I still get that even though I’ve done more than 300 podcast episodes, I’ve written a book, I still feel like a bit of an impostor, because I kept remembering the person that I was before stroke. And I was, and I wasn’t not this kind of guy. Like I didn’t do anything public. You know, I wasn’t out there. And I still feel like my identity hasn’t caught up with all the stuff that I’m making it do, that it hasn’t signed up for.
Jenn Williams 52:33
Yep, I absolutely understand that.
Bill Gasiamis 52:37
And I don’t even know why I’m doing it all sometimes, why the hell am I doing? Why am I doing my 300 and 10th podcast episode that’s like.
Jenn Williams 52:48
I can tell you why. Okay, number one, it’s fulfilling to help other people, just in general. Number two, there is such a lack of voices and information around brain injury. So you’re making an impact by spreading information. And number three, it’s healing to connect with other people that have gone through what you’ve been through,
Bill Gasiamis 53:11
Tick, tick, tick. That’s exactly why.
Jenn Williams 53:18
Because I do the same thing I’m always looking for, like, how can I make an impact? How can I, you know, help this person? What resource do they need? That’s my same drivers as well.
Bill Gasiamis 53:31
And sometimes I feel incapable of actually helping and making an impact. And because a friend of mines daughter had a hemorrhagic stroke last year, and she was 17, at the time, I was in ICU with him. And you know, we struggled together. They’ve come a long way, and she’s a lot better, but she’s got pain now in her left foot.
Bill Gasiamis 53:58
So when things started to settle down, the numbness turned to pain and the pain kicked in. And she’s struggling.
Jenn Williams 54:09
How long ago was it?
Bill Gasiamis 54:13
It was in the last 12 months. And now she’s struggling dramatic pain, because of where the stroke happened was the area of her brain where pain receptors do that work, right? That’s as much as I know about it.
Jenn Williams 54:29
Was it the thalamus?
Bill Gasiamis 54:32
It was in the middle of the brain near the very center of the brain. Right side, when you see the brain scans, you see the two sides of the walnut and then in the middle, there’s kind of like a bit of a gap. The bleed was from the right side, she had an AVM that damaged the right side, but it bled into that gap between the two pieces of the walnut.
Bill Gasiamis 55:01
Anyhow, they drained it and she’s got an amazing result, right. But she’s got this pain now. And that’s the thing. It’s like for me, I realized the works not done. And I don’t know how I don’t know how useful it is this podcast to people who haven’t had who have pain who feel debilitating pain.
Bill Gasiamis 55:23
And I can’t relate to it because I didn’t feel that I feel a little bit of pain, but not ridiculous. She’s not able to sleep because of it, and it’s causing some drama, so that I feel I still feel like I’m not doing enough, like, my work is inadequate.
Jenn Williams 55:40
Because every injury is different. I used to hate that phrase, that every brain injury is different. But I’ve learned to accept it and actually appreciate it. Because that means that you’re not pigeon holed into one recovery timeline, or whatever it may be. So even though you might not relate to her on the pain level, the general concept, you know, is all very similar.
Bill Gasiamis 56:16
And I’ve seen that other side of what stroke does to families, because she’s got great parents, and they’re doing a good job, and it’s all good. But I can see the strain on the family, and the mom and dad and what they are going through. And then I just think about that. So it’s on my mind a lot more.
Bill Gasiamis 56:39
And I’m getting a little bit overwhelmed by it, not in the it’s not going to shut me down or stop me from doing what I’m doing or anything. But you know what, my heart goes out to them. And that’s what it is. And I just don’t want them to be in that situation. And I hope that they have a result a resolution and they’re going after every possible resolution, you know.
Bill Gasiamis 57:01
So, yeah, it’s just man and this guy, this guy I grew up with. I’ve known him since I was about four years old. And he is a radiographer, I wrote about him a little bit in the, in the acknowledgments in the back of the book. And he helped me out with all the brain scans that I did so he and his team would be taking my brain scans at the hospital that I was at, at the Royal Melbourne Hospital.
Bill Gasiamis 57:31
And he wasn’t meant to, but he would come after the scan and go, it’s looking alright, or because I was I had about eight or nine MRIs in the time that they were monitoring the blood vessel that burst the AVM and he would come and go, it doesn’t look like it’s changed, things have settled down a little bit, etc.
Bill Gasiamis 57:52
And stopped me from waiting about one month to get the news with my doctor. So that was really cool. And then to be in the damn hospital ICU with his daughter on life support because of this same issue that I had 11 years later, it’s just crazy. I just can’t comprehend it. But it was great to be that guy that was able to walk in the ICU and show them what is possible. Without saying anything. All I had to do was walk in there.
Jenn Williams 58:38
Can I ask you a question? Have you seen any gains or changes as you’ve gotten farther away from your injury?
Bill Gasiamis 58:52
Yep. Cognitively, things are improving still. And physically things are stable to slightly declining. But the decline is not something that I can address. So what I noticed is my balance gets worse sometimes. And my pain and the tightness and the spasticity in my left side gets a little bit worse. Now again, nobody would know.
Bill Gasiamis 59:31
If I said that to somebody that knew what spasticity looked like. For some stroke survivors. That would go you don’t have spasticity. But the feeling that I have has sometimes, sometimes gets worse. And recently I kind of smiled when I said recently I fell off a ladder. And the reason When I fell off the ladder was because my left hand gave away it just let go of the ladder. And that does happen from time to time. And usually it lets go of a bottle that I’m holding or my telephone.
Jenn Williams 1:00:12
I had that happened with my purse last week. I was really tired, I was holding my purse and my hand just let go.
Bill Gasiamis 1:00:22
Yep. I’ve lost the phone because of that. All sorts of things. But then this time, I was climbing a ladder, I was only two rungs up, I was going up to the third rung. And my left hand just let go.
Jenn Williams 1:00:39
Thank goodness, you weren’t further up?
Bill Gasiamis 1:00:41
Well, I still fell backwards. And I fell onto a middle bar, a scaffold bar. Because my full time business is we have a property maintenance company. And in order to do the repairs on this particular home, that we’re working on, I got a scaffold so we could be safe.
Jenn Williams 1:01:06
The irony.
Bill Gasiamis 1:01:07
Yeah. So I’ve fallen off the ladder backwards onto one of the horizontal scaffold bars that are holding the construction of the, you know, all the poles together, it broke my fall, I landed on my ribs. And then and then I fell another three feet, or a meter to the deck below and hit my head. So it was quite a shock to find myself down there. And then I couldn’t sleep properly for about a week. And then I started to sleep better after that.
Bill Gasiamis 1:01:43
And it’s been around three weeks, and only for the first time last night, I was able to lay on my side, haven’t been able to do that for three weeks. Because of the pain, I got it checked out. There was a lot of bruising, there was no broken bones or anything. But that is not an escalation of my condition. It’s kind of what my condition is doing.
Bill Gasiamis 1:02:07
And I think what it’s doing is it needs more TLC, it needs more therapy and more rehabilitation, I’ve been going to the gym trying to strengthen my left side. And I still, you know, eat well, and all those things, try and get as much sleep as I can. But I think my left side is becoming more needy, and I’m not putting enough effort in. And it feels a little bit number.
Bill Gasiamis 1:02:41
And maybe, and in winter, it always gets worse. It’s getting into the winter months now. We’re first day of winter today here for us. June the first and and I think in winter, my sensation decreases on my left side, it gets more colder and more numb. And I remember now that you asked me thanks for asking this because it’s just reminded me everything my mum,
Bill Gasiamis 1:03:06
I was at my mom’s the other day. And I was in her way. And she was just trying to not interrupt my conversation and kind of squeezed through him. But I wasn’t paying attention I didn’t notice. So she went to pinch me on my bum. And she said, Why aren’t you moving out of the way? And why aren’t you responding? I said to what? Because I’m pinching you on the bum. I can’t feel it. She says really? She thought I was joking, and that I was just putting up with it. I couldn’t feel it at all. I had no idea she was doing it. So yeah, those types of things are happening now.
Jenn Williams 1:03:48
Have you heard of something called post stroke? recrudescence? No, do tell this is my favorite topic. You’re gonna love it. Um, so there’s been there was a study done at Massachusetts General in I believe it was 2016 or 2017. And then the American National Institutes of Health just did a study on it, I believe last year.
Jenn Williams 1:04:14
So the basic explanation how this was explained to me is that when you have a brain injury, and you have neurons that die, the neurons around the dead ones, eventually pick up the job of the dead your neurons as their second job. Well, if your body feels like there’s a crisis, which in the body or crisis can be that you’re tired that you’re stressed. It could be you have low blood sugar, the brain can say, oh crisis, we need to focus on our first job and it stops doing the second job.
Jenn Williams 1:04:53
So I have symptoms that flare up. When I’m really stressed when I haven’t slept At if my I didn’t really have blood pressure or blood sugar issues, but you know, things like that that could be considered a crisis in the body. And my brain goes, Nope, we’re not doing those things. So my hand stops working, I get tingling in my hand tingling in my face tingling in my foot, my balance goes, I get vertigo, all these other symptoms, and it can feel like another stroke or it can feel like just after my stroke.
Jenn Williams 1:05:28
So I’ve gone to the ER before, just to make sure I get checked to make sure that something else isn’t happening. And I’m usually fine. But I learned about that. And it made so much sense. And when I talked to other survivors about it, they go, oh, yeah, when I’m tired, all my symptoms crop up. When I’m really stressed about dealing with my doctors, all these symptoms pop back up. So it might not be necessarily decline. It could just be you’re not at homeostasis, for lack of a better word.
Bill Gasiamis 1:06:03
I love that explanation. I think that’s also is valid. What you just said is definitely valid. Classic example is if I have an argument with my wife. Happily married for 19 or 20 years. So I get more symptoms. Yes. So when that I’m in emotional, negative emotional state, I get more symptoms. And it encourages me not to be there for too long. And I’m getting better at not staying angry or mad for ever, and ever. So there’s that. I agree with that. That does happen. And I’ve said it a few times on the podcast. And when I eat the wrong food.
Bill Gasiamis 1:06:56
For me it’s like, say a pastor, or a sugary drink or something like that. Oh, my gosh, things just get so much worse. Brain fatigue, fog, tingling, balance, everything kind of just gets worse. So I agree with what you’re saying. I may have. And that’s a thing, because it’s happened recently a number of things have happened that have bugged me that have made me think but going to the mind goes to maybe it’s getting worse.
Bill Gasiamis 1:07:26
I don’t know that it is I’m not It’s not stopping me from doing anything. Although I am very cautious about letters. Always have been even though I fell from one, I always have been. Yep. And what it says to me is I just need to go and get more rehab, more therapy. That’s all it says. And I’ve been at massless chiropractors, this guy that I’ve been there the whole time. And they know me really well. So yeah, I don’t know. It’s always changing. And I’m always adjusting. And I’m always finding a way, a way to overcome it.
Jenn Williams 1:08:09
I do think that learning about the poststroke recrudescence helped me to be more self aware. Because when I have those symptoms flare up, I can take a step back and go okay, what does my body need right now? Did I get my electrolytes today? Did I take my medications? Maybe I forgot my medications. You know, maybe I forgot my aspirin or you know, whatever. How did I sleep last night? Am I stressed? Do I need to go move my body like so it gives me that pause to kind of have a little self evaluation to see where I’m at.
Thalamic Stroke Recovery: Insomnia Causes And Solutions
Bill Gasiamis 1:08:50
Yep, I love it. I agree with that. That’s what I do every time I hit a wall, that wall is just the just have a wrist wall? Or is this the do something more than wrist wall? Like what is it? What do you have to respond to? So yeah, for me for work, because I’ve got a couple of guys working with me, I’ve got a business partner. I could just say, I’m not coming in. I need not to be there. And then I won’t be there. That’s been a good thing that I’ve been able to do. Of late. Tell me about your insomnia a little bit. So is it insomnia that had begun after all your medical issues? So what’s it like? How did it begin? Can you describe it? Explain it?
Jenn Williams 1:09:40
Well, you know, when you talk about insomnia with your doctor, they’ll ask you is it that you have trouble falling asleep or you have trouble staying asleep? For me, it’s both I have trouble falling asleep and staying asleep. And I actually didn’t realize I guess that it was insomnia at first but cuz I was so fatigued all the time, I just figured that I was just fatigued.
Jenn Williams 1:10:05
And I was talking to my counselor, and I can’t remember what did I say? I said, I said, I can’t get out of bed. I’m exhausted, and I’m so frustrated. I must be depressed, blah, blah, blah. And he said, Well, depressed people aren’t frustrated about it. So that’s probably not it. I said, Oh, okay. And he said, How have you been sleeping? And I went, Oh, not well, no.
Jenn Williams 1:10:35
And I push, I learned this probably a year or two after my injury. And I was trying to take care of it on my own and trying to take melatonin and trying to just adjust my life around my sleep schedule, and all these other things, and it wasn’t working. So I eventually got a in lab sleep study in Boston. And they said, Yeah, you have sleep latency, your cycle has shifted. So you just need to adjust your life around your new circadian rhythm.
Jenn Williams 1:11:14
Well, that’s semi practical, that’s not extremely practical. So I talked to my primary care and gave me some prescriptions and tried a bunch of different ones. And I eventually started seeing my naturopath for something else. And we got that addressed. And she said, Is there anything else you want me to help you with? I said, Well, if you could figure out my sleep, that’d be great.
Jenn Williams 1:11:43
And she said, Sure, we did some adrenal testing. And it turns out that I was making melatonin at the wrong times a day. And I had like, no cortisol. And then I found out, yeah, for those of you that don’t know, a lot of people think that cortisol is the stress hormone, but it’s actually the counterpart to melatonin. So it’s what wakes you up in the morning, it’s what keeps you going through the day.
Bill Gasiamis 1:12:05
So the too much cortisol can be stressful. Yes, cortisol is necessary, because it’s, it’s the wake up hormone, it’s the wake up part of the sleep cycle, the thing about it is is, once it kicks in, you want to see it drop off, after it’s got you awake, you want to say drop off, and then at the end of the day, when the sun starts coming down, you want to say cortisol, not be there. So that right, melatonin, can start doing its job of putting your body into the sleep cycle.
Jenn Williams 1:12:42
So I was I had very little to almost no cortisol in the morning, your cortisol levels supposed to be like at a 25. And I was at a three. And then the afternoon, you’re supposed to be between like a five and a 10. And I was point five. And I was also getting a melatonin spike in the afternoon. So my melatonin would jump really, really high at like three o’clock in the afternoon.
Jenn Williams 1:13:07
So my hormones were all messed up. Another side note, I realized through doing my own research through all of this, that more than half of brain injury survivors have some sort of adrenal dysfunction, which is where your cortisol and your melatonin is produced. So we did this adrenal test, found this out. And I’ve been using different medications to kind of retrain my adrenals.
Jenn Williams 1:13:37
I used to sleep until noon. And now I get up at like 830. And that has taken me a couple years to force yourself to retrain and like get up at seven o’clock in the morning and take my cortisol so that it produces at the right time. Ah, yeah, I don’t have to take it anymore. My body has figured out the cortisol part. So now I’m working on the melatonin part. But I feel so much better.
Jenn Williams 1:14:07
Even though my sleep is still very broken. I sleep for like three hours, I’m up for a little bit and I sleep for three hours. But I’m getting more restful sleep, and I have that natural waking cycle that’s supposed to happen. So it’s been a very long journey. On the insomnia piece.
Jenn Williams 1:14:26
I’ve done all of the healthy sleep habits, no technology, two hours before bed, listening to delta waves, meditating, reading, you know, dim lighting, essential oils, all these things to try and create this like almost romantic sleep situation. And it really was just my adrenals that needed to be retrained. So it’s been a very long process but it is worth it.
Bill Gasiamis 1:14:53
I love it because you have got a positive outcome and that just goes to show you it is something that you can address And it’s whether they’re looking Yes, deeply enough into it. When I typed in cortisol deficiency into Google, it says, cortisol deficiency occurs when the adrenal glands do not produce enough cortisol, this can happen for four main reasons when the pituitary gland is unable to produce the chemicals needed to tell the adrenal glands to switch on the cortisol production. So it’s, it’s a proper brain communication signaling issues. So what I why I read that was if anyone’s struggling with this sleep is to ask the big questions beyond kind of have a sleep medication.
Jenn Williams 1:15:48
I didn’t want to be on sleep medication. I didn’t want to be on that crazy stuff for years and years. I wanted to fix it. And you know, instead of just saying, I don’t know, I don’t sleep well. Give your doctor details. Explain, I’m not falling asleep while I’m waking up every 30 minutes, because that’s what I was experiencing, I was waking up every 30 minutes, and I would be up for an hour, hour and a half. And it was like naps, all day naps, because I was still out of balance. So asking the very detailed questions and being very open about what you’re experiencing can really make a difference.
Bill Gasiamis 1:16:28
Get your pituitary gland checked out, get your adrenal glands checked out, get your thyroid checked out. Don’t just leave it at an some medications sleep because I’m not sleeping properly.
Jenn Williams 1:16:44
And I had a thalamic stroke, which I have since learned, because I did not know this that the thalamus is the distribution center of the brain. So all of the information that comes in, goes through the thalamus and then gets sent out. So when you have damage to your Thalamus, it can affect everything. Because the thalamus communicates with everything. So it could depend not even your pituitary. It could be the lambic issue, it could be any number of things.
The Hardest Thing About Stroke For Jenn Williams

Bill Gasiamis 1:17:15
Yeah, yeah, it’s important to know where the stroke happened and what part of the brain is impacted. And what that part is, does for a living, you know, how it pays its rent. So that’s awesome. I’m glad you’re getting a result and you’re seeing an improvement. As we come to wrap it up, tell me a little bit about what the hardest thing about stroke for you was?
Jenn Williams 1:17:42
Ah, I would say grief, the grieving the loss of my old life. And my old identity, I realized that I had really begun to absorb a strong, deep work ethic as my identity. So when I couldn’t work, I didn’t know who I was. I was like, I don’t, I am not working 80 hours a week, and busy and all those other things like I don’t know myself. And I had to grieve the loss of that old life.
Jenn Williams 1:18:22
And I still have days where I cry, and unlike what happened in my old life. And you know, the the loss of some relationships, there are, you know, you were talking about the family thing earlier, my family’s wonderful, but I do have some family members that have never really asked me about my brain injury that have never shown any curiosity and how I’m doing which is eye opening.
Jenn Williams 1:18:56
And then I have friends that just couldn’t handle it, they just could not handle the fact that I was on this road to recovery. And, you know, wasn’t just accessible to them 24 hours a day or anything like that. So I think just in general grief is a is a really huge part of it. And I think that’s the hardest part for me was the grief.
Bill Gasiamis 1:19:20
The loss of identity is very interesting one I speak about that in my book as well. I think it’s chapter three. And the good part about that is you can rehabilitate your identity really quickly. Yes, that’s a good part about it. You can become involved in all those things that you’re become involved in to keep you busy for another 80 hours a week, but just in a different way. And you pick up relationships in those new spaces, just like you were interacting with people in those old spaces. So that’s really cool.
Bill Gasiamis 1:19:59
The friends one is an interesting one, because many stroke survivors experienced the same thing. It says more about the people who kind of step away or don’t know how to handle it than it does about you. And I think it’s a blessing that they move away and step away.
Bill Gasiamis 1:20:23
Because if they’re incapable of supporting you, or being okay, or normal, or just be there, they’re incapable of doing that, then I think that would make your recovery harder, it would cause some stress or some aggravation, or whatever. And I think they do a really good job of going. I don’t know what the hell I’m doing here. I’m out of it. I’m gone. It seems weird, and it seems like a bit of a letdown and that they’re not doing what you would expect of them. But I think they’re doing the best thing they could possibly do. And that’s like, go away.
Jenn Williams 1:21:02
I mean, if that if that would be hard for them, then I don’t want them to be present. That’s not fair to either of us. I do also want to just talk a little bit about gratitude. I, my counselor asked me one day, he kind of said, Oh, I bet if you could go back in time and change it, you would. I thought about it. And I said, No, actually, I wouldn’t. And he said, Okay, you got to explain that to me. And I said, I have met people that I never would have met. Without being on this journey. I’ve connected with people.
Jenn Williams 1:21:47
And it changed me for the better. I have more internal peace. I don’t feel the need to push myself to work 80 hours a week anymore. I’m happier. I appreciate so many little things. Every day, I write down three things that I’m grateful for. And sometimes I’m grateful that I have really nice sheets on my bed. That’s okay. And I never would have had that much gratitude prior to my injury.
Bill Gasiamis 1:22:19
I relate to that. That’s why I wrote a book called The Unexpected Way That A Stroke Became The Best Thing That Happened. And people think I’m mad.
Jenn Williams 1:22:25
I know. I saw your title. And I was like, yes.
Bill Gasiamis 1:22:32
People think I’m mad. And it’s like, I’m not saying anything positive. Although there is positive things. I’m not saying that pain is good. And all this is like, we should suffer indefinitely. And it’s suffering is amazing. With a purpose it’s okay. It’s manageable. Yeah. Suffering, and then you convert it into a purpose, like a podcast, or helping other people at a homeless shelter or whatever. Like it transforms. I can’t explain how, but it just does.
Bill Gasiamis 1:23:07
And it makes it less shit. And then that’s all I want. I want it to be less shit than it was yesterday. And if it is, then that’s okay. And yeah, it’s like, I don’t know, I would love to learn the lessons without going through stroke. But it didn’t happen that way. I wasn’t that wise, I wasn’t that intelligent.
Jenn Williams 1:23:36
We apparently had to get some knocks in the head to get the point across.
Bill Gasiamis 1:23:42
A bit thick in the head. So it’s something needed to change, maybe a bolt of lightning or something or jolt or something. It’s just intensely crazy that you would say that that you would say I wouldn’t change it. I have met so many people that wouldn’t change. What happened to them? It’s just crazy. And it’s counterintuitive. What is something that stroke taught you? Did I already ask that?
Jenn Williams 1:24:19
I don’t think so. If you did, I forgot and we’ll say it again. Ah, gosh, something that stroke has taught me? It has taught me so much. I guess it’s hard to pinpoint one thing. I would say probably the gratitude piece obviously that’s a big part and then the it’s okay to advocate for yourself. It’s okay to ask questions about your health care. And I say It’s all the time and some people don’t like it, but your doctors or your employees, you can fire them.
Jenn Williams 1:25:05
If it’s not working, it is not working, and you can move on to the next. And that has been a huge change for me to say, You know what, this isn’t a good relationship, I’m moving on to the next person. And just having the self awareness and the comfort in saying that brings a whole new depth to self-advocacy for me internally, in all aspects of my life, it has taught me to stand up for myself in critical moments that I really need to.
Bill Gasiamis 1:25:41
That’s profound. It’s so good to stand up for yourself, and to take them on, and to just make them accountable. That’s all. That’s all you’re doing. Just checking out the information they’ve given you is accurate, and it’s applicable to you. And it’s the right information. It’s no different to what they do to you, when you get asked by 25 different health professionals in the hospital. What happened to you? So what happened to you? It’s on the chart, read the chart, but tell me what happened to you.
Jenn Williams 1:26:17
I told your nurse, I told this person, I said it in my last appointment.
Bill Gasiamis 1:26:23
Yeah. And it’s just what they’re doing is they’re double checking that they’ve got the right person in front of them that they are talking about the right and that’s all we need to do is okay. Okay, so what are you going to do about it? How you can help me? Why are we doing this? What’s the purpose of that? Why aren’t we doing this? Why aren’t we doing that? And you can do it nicely, you can have a lovely conversation with one of your medical professionals. If they don’t like it, that answering questions, well, then they’re the wrong person, and then you should fire them and you should move on and get somebody to help.
Jenn Williams 1:26:53
And I had one neurologist that my first appointment with her she was the other neurologist had left the practice and they had someone new. And during my appointment, she kept looking at her smartwatch. And she was like giggling, and so she was clearly reading messages on her smartwatch. And I got home, I was so angry. And my husband was like, try talking to her about it. Just try talking to her about it.
Jenn Williams 1:27:22
She’s new to the area, she’s the only one in the area. So see if you can work it out with her. And my next appointment, I said, I need to tell you that at my last appointment, I did not feel like you were as invested in my care as I am. And I really need us to be on the same page. And she sat right up and I’m like, oh, oh, I’m so sorry. I didn’t mean to do that.
Jenn Williams 1:27:45
Blah, blah, blah. And we had a great relationship until she moved again, gone through a lot of neurologists, but even just saying that, in my previous life, I would not have said that. I wouldn’t have ever said something like that. But I did. And it worked out and we got on the same page. And we took steps for my recovery. And it felt very collaborative. So even just saying something like that made a huge difference.
Thalamic Stroke Recovery, Grief, And Resilience
Bill Gasiamis 1:28:16
Excellent. What would you like to say to some of the stroke survivors that are listening, that are just on their journey or a few years down the track? Things are a little bit challenging for them? What do you want to say to them?
Jenn Williams 1:28:33
Recovery is not a sprint. It’s a marathon. It is not three months, it is not a year, it is not two years. It is a life altering journey. And I will tell you, I probably spent the first three years of my recovery and grief. And once I got through all of that I was able to give back. I was able to start helping people and speak at support groups and do self advocacy work. And there’s a lot of really beautiful things that can happen on the other side of that grief. You just have to hang in there.
Bill Gasiamis 1:29:13
Thank you so much for joining me on the podcast. I really appreciate it.
Jenn Williams 1:29:20
Thank you. It was really nice to be here. I really appreciate it. I love talking about brain injury.
Bill Gasiamis 1:29:26
Me too. You wouldn’t have guessed from the 310 episodes. But yeah, I don’t mind that either. Thanks so much, Jen.
Jenn Williams 1:29:40
Thanks, Bill.
Bill Gasiamis 1:29:42
Thanks for joining us on today’s episode. If you are interested in a copy of my book about stroke recovery. You can grab a copy on Amazon by visiting on Amazon or by visiting recoveryafterstroke.com/book to learn more more about my guests including links to their social media and to download a full transcript. Head over to recoveryaftershow.com/episodes.
The post Thalamic Stroke: Symptoms, Treatment, and Recovery appeared first on Recovery After Stroke.
301 قسمت
Manage episode 426580023 series 2807478
Comprehensive Guide to Thalamic Stroke: Symptoms, Treatment, and Recovery
Introduction
Thalamic stroke is a type of stroke that affects the thalamus, a small but critical structure deep within the brain. The thalamus plays a crucial role in relaying sensory and motor signals to the cerebral cortex and regulating consciousness, sleep, and alertness. Understanding thalamic stroke is essential for patients, caregivers, and healthcare professionals to ensure prompt diagnosis, effective treatment, and optimal recovery.
Understanding Thalamic Stroke
What is a Thalamic Stroke?
A thalamic stroke occurs when the blood supply to the thalamus is interrupted, leading to tissue damage and loss of function in this vital brain region. The interruption can be due to an ischemic stroke, where a blood clot blocks a blood vessel, or a hemorrhagic stroke, where a blood vessel bursts and causes bleeding in the brain.
Symptoms of Thalamic Stroke
The symptoms of a thalamic stroke can vary widely depending on the specific area of the thalamus affected. Common symptoms include:
- Sensory Disturbances: Numbness, tingling, or a burning sensation on one side of the body.
- Motor Impairments: Weakness or paralysis, typically affecting one side of the body (hemiparesis or hemiplegia).
- Pain: Thalamic pain syndrome (Dejerine-Roussy syndrome), characterized by chronic pain on the side of the body opposite the stroke.
- Cognitive and Emotional Changes: Memory problems, confusion, emotional instability, and difficulty with attention and concentration.
- Vision Problems: Partial or complete vision loss, or visual field deficits.
Causes and Risk Factors
The primary cause of thalamic stroke is the obstruction of blood flow to the thalamus. Risk factors include:
- Hypertension: High blood pressure is the most significant risk factor for stroke.
- Diabetes: Increases the risk of blood vessel damage and stroke.
- Atherosclerosis: The build-up of fatty deposits in the arteries can lead to clot formation.
- Heart Disease: Conditions such as atrial fibrillation can cause blood clots that travel to the brain.
- Lifestyle Factors: Smoking, excessive alcohol consumption, obesity, and lack of physical activity.
Diagnosis of Thalamic Stroke
Diagnostic Procedures
Early diagnosis of thalamic stroke is critical for effective treatment. Diagnostic procedures include:
- Physical Examination: Neurological assessment to evaluate sensory, motor, and cognitive functions.
- Imaging Studies:
- CT Scan: Quickly identifies bleeding in the brain.
- MRI: Provides detailed images of brain structures and can detect smaller strokes.
- Blood Tests: Evaluate overall health and identify risk factors such as high cholesterol and diabetes.
- Electrocardiogram (ECG): Detects heart abnormalities that could lead to stroke.
Treatment Options for Thalamic Stroke
Acute Treatment
Immediate treatment aims to restore blood flow and minimize brain damage:
- Thrombolytic Therapy: Clot-busting drugs such as tPA (tissue plasminogen activator) are administered within the first few hours of an ischemic stroke.
- Endovascular Procedures: Mechanical thrombectomy to remove a large clot in cases where thrombolytic therapy is ineffective.
- Surgery: In cases of hemorrhagic stroke, surgery may be necessary to repair damaged blood vessels and relieve pressure on the brain.
Rehabilitation and Recovery
Rehabilitation focuses on restoring function and improving quality of life:
- Physical Therapy: Exercises to improve strength, coordination, and mobility.
- Occupational Therapy: Assistance with daily activities and strategies to adapt to physical limitations.
- Speech Therapy: Helps with communication difficulties and swallowing disorders.
- Pain Management: Medications and therapies to manage chronic pain from thalamic pain syndrome.
- Psychological Support: Counseling and support groups to address emotional and cognitive changes.
Prognosis and Long-term Outlook
The prognosis for thalamic stroke varies based on the severity of the stroke and the promptness of treatment. Many patients experience significant recovery with comprehensive rehabilitation, although some may have lasting impairments. Regular follow-up care and management of risk factors are crucial for preventing recurrent strokes.
Prevention Strategies
Lifestyle Modifications
Adopting a healthy lifestyle can significantly reduce the risk of thalamic stroke:
- Healthy Diet: Rich in fruits, vegetables, whole grains, and lean proteins.
- Regular Exercise: At least 150 minutes of moderate-intensity exercise per week.
- Smoking Cessation: Quitting smoking reduces stroke risk.
- Alcohol Moderation: Limiting alcohol intake to moderate levels.
Medical Management
Managing underlying health conditions is essential for stroke prevention:
- Blood Pressure Control: Regular monitoring and medication adherence.
- Diabetes Management: Keeping blood sugar levels under control.
- Cholesterol Management: Medications and dietary changes to lower cholesterol.
- Anticoagulant Therapy: For patients with atrial fibrillation or other heart conditions.
Conclusion
Thalamic stroke is a serious medical condition that requires prompt diagnosis and treatment. Understanding the symptoms, risk factors, and treatment options can significantly improve outcomes for patients. With comprehensive rehabilitation and lifestyle modifications, many individuals can achieve substantial recovery and improve their quality of life.
Thalamic Stroke Recovery Interview with Jenn Williams
Jenn Williams discusses her thalamic stroke recovery, the risks of the contraceptive pill, and the importance of self-advocacy and resilience.
Instagram
Recrudescence of Deficits After Stroke
Middle People Project
Brain Injury Association Of America
Highlights:
01:52 Introduction
02:48 The Beginning Of Thalamic Stroke Recovery Journey
16:20 Self-advocacy For Medical Care
35:36 Post Thalamic Stroke Recovery And Deficits
43:02 The Middle People Project
51:47 Pain Management And Personal Growth
1:08:50 Insomnia Causes And Solutions
1:17:14 The Hardest Thing About Stroke
1:28:16 Thalamic Stroke Recovery, Grief, And Resilience
Transcript:
Bill Gasiamis 0:00
This episode of the podcast is brought to you by headbed.com.au. Hey everyone. Before we dive into today’s episode, I wanted to share something special. In Episode 305, I interviewed Catherine Randabel, the inventor of HeadBed, a product revolutionizing hair salons, especially for stroke survivors.
Bill Gasiamis 0:21
The HeadBed provides excellent neck and head support during hair washes, reducing strain and promoting better blood flow. For stroke survivors. This means lowering the risk of arterial damage and easing concerns about another stroke. It ensures a safe and enjoyable salon experience and I’m thrilled to support a product that aligns with my mission of stroke prevention and safety.
Bill Gasiamis 0:47
In our interview, Catherine explained how the HeadBeds ergonomic design prevents neck hypertension, a common issue increasing stroke risk. With the HeadBed you can feel confident and comfortable at the salon knowing your health is prioritized.
Bill Gasiamis 1:04
If you’re a stroke survivor or know someone who is HeadBed is a must have for your next salon visit, check out episode 305 for my full interview with Catherine and learn how this product can make a difference. For those in the United States visit head bedusa.com to get yours today and to enjoy peace of mind at the salon.
Bill Gasiamis 1:27
Now I’d also like to mention my book, The Unexpected Way That A Stroke Became The Best Thing That Happened. 10 tools for recovery and personal transformations. If beaches inspiring stories from 10 stroke survivors and offers hope for those on the road to recovery. For more information visit recoveryafterstroke.com/book or search for my name Bill Gasiamis on Amazon.
Introduction – Jenn Williams

Bill Gasiamis 1:52
Now this is episode 309. And my guest today is Jenn Williams, who at the age of 33 experienced a left thalamic ischemic stroke. In this compelling episode, Jenn shares her incredible journey of thalamic stroke recovery, detailing the early symptoms and the misdiagnosis. And the moment her life changed forever.
Bill Gasiamis 2:14
Jenn also discusses the emotional and physical challenges of recovery, the risks associated with taking the contraceptive pill, and the importance of self advocacy. She highlights the impact of gratitude, community support, and how she has turned her experience into a mission to help others through her work with the Brain Injury Association and The Middle People Project. Jenn Williams, welcome to the podcast.
Jenn Williams 2:41
Thanks for having me.
Bill Gasiamis 2:43
Thank you for being here. Tell me a little bit about what happened to you.
The Beginning Of Thalamic Stroke Recovery Journey
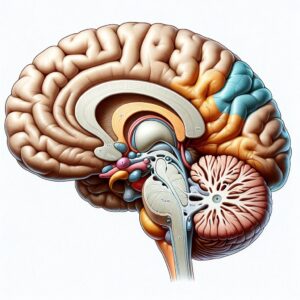
Jenn Williams 2:48
So it was 2016. And I was working as an insurance agent in a busy office and my wrist and my hands on my right side kind of got that feeling like it was falling asleep while I was at work. And I kept trying to shake it out like you do when your arm falls asleep or something and it wasn’t working. I made a very poor joke now looking back to my coworker and said if I die, this is how this started.
Jenn Williams 3:19
Yep. So the next day, I had that same tingling in my foot on the same side and half of my face. So I got into see my primary care. And she said, you know, we’ll run some blood tests, it could be a mineral deficiency, you know, all this other stuff. There was some miscommunication on what the tests were supposed to be.
Jenn Williams 3:45
So I went in and out a few times. I believe that was a Tuesday when that all started. And then by Friday of that week, the tinkling was my whole right side. So I had a follow up the following Thursday, and my husband was meeting me at the appointment, he was taking some time off from work, because we didn’t know what’s going on and I wanted some support.
Jenn Williams 4:08
And I drove from my house to the appointment. And by the time I got there, I didn’t feel good at all. I don’t feel right, my stomach is turning, I’m dizzy. I went to go get out of a car and I fell onto the hood of the car and my husband was like what is happening right now? We went into the appointment and she said, we’ll order some tests. You know, we’ll give you a call and let you know.
Jenn Williams 4:35
And during this appointment, my husband called his mother to come get my car because I said I don’t feel safe driving. There’s something going on. And in the 10 minute ride that it took to go from the doctor’s office to my house I was paralyzed. And I don’t know about you but I was raised to believe you know the doctor is the end all be all.
Jenn Williams 4:58
That’s what they do. That’s what they you know, you believe what they say. So I looked at my mother in law, and I said, It’s okay, I’ll just wait for the doctor. And she screamed and said, This is not okay. And she took me to the ER. And they found that I had had a left thalamic stroke, ischemic so clot.
Jenn Williams 5:22
And I was in ICU for about three days, they wanted me to go to inpatient rehab. But my family and friends were like, we’re not doing that we’re not going to do inpatient, we’ll just help you at home. So I was fortunate enough to go home after leaving the ICU. And I had a lot of support for those three weeks.
Jenn Williams 5:41
But as many brain injury survivors know, there’s a lot of tests and things that proceed after that. And there was no real issues that they could determine no clotting disorder, no high blood pressure, no diabetes, nothing like that.
Jenn Williams 6:00
So the general idea is that it was caused by medications, I was taking contraceptives and migraine medications, which both have those dangers, and family history, there is some family history. So definitely not what I expected in my life, at age 33. At the time. But it’s been a really educational incredible experience.
Bill Gasiamis 6:26
Yeah, you know, you’re not the first person I’ve interviewed who was taking a contraceptive. There’s, I dare say there’s at least another two or three and younger as well, kind of in their 20s. And what’s interesting is when I asked them did you know about that risk? They all said no.
Bill Gasiamis 6:54
And even if they did, no, I’m not sure that it would have changed anything if they were told, by the way, this medication has this risk, but I don’t know if it would have changed anything. Because I know sometimes contraceptive pill is taken for non contraceptive reasons. Yeah, so were you aware that it was a risk that came with taking the contraceptive pill?
Jenn Williams 7:24
Yes, I didn’t know I started when I was in high school. And I didn’t realize at that point, but then as I got into adulthood, I started reading those packets that they give you when you leave the pharmacy. And I honestly, I think it was one of those things where I said that’s for old people. That doesn’t happen to young people.
Jenn Williams 7:43
That’s not going to happen to me. And, you know, I was on contraceptives for 25 years. And I just assumed it wasn’t going to happen to me. Yeah, but I can I kind of go on a tangent. Is that okay? One of my biggest frustrations, this whole process has been the realization that a significant percentage of the population has clotting disorders.
Jenn Williams 8:13
And we just prescribe medications, especially contraceptives, we just prescribe them to young girls, and we don’t check for those things. And that makes me so scared for our general population, but scared for like my nieces. That I mean, that’s a horrible. I mean, yes, I’m grateful for it in so many ways, but it is a really horrible experience. And I don’t wish that on anyone. And I don’t understand why we don’t check people for things like that. Before we prescribe medications.
Bill Gasiamis 8:44
I love that because that’s the biggest issue is these know, what’s the word? There’s no kind of investigative work done. Yeah. Before somebody says you should take this. I mean, I know even my father in law, who’s in his 80s. He’s on like, 55,000 medications. But when even though he’s on so many, nobody still does the whole, I wonder if this is going to be appropriate for you to take because that might interact with that and that might do that and that.
Bill Gasiamis 9:18
And my wife, she’s a bit of a how can I describe her? She’s a bit of a like a detailed freak, like she does details about things that most people would just roll their eyes out, right? It’s just her nature. She’s very thorough, and all that type of thing. And if it wasn’t for her dad would be taking medication that instead of lowering his blood pressure is making it worse or you know, they’re giving him stuff that works with the blood pressure medication to lower even further.
Bill Gasiamis 9:57
And she’s the one doing the research and he’s been in the system forever. And and it’s really scary to be a family member and to put all your trust in the medical system and not question it. I think that’s kind of a little bit of putting your head in the sand kind of scenario. And I was trained like that as well, when there was something wrong. My parents took me to the doctor, and whatever the doctor said, what we did, and thankfully, all worked out well. But if I took that approach, when I went to hospital for my first bleed.
Intro 10:35
If you’ve had a stroke, and you’re in recovery, you’ll know what a scary and confusing time it can be, you’re likely to have a lot of questions going through your mind, like, how long will it take to recover? Will I actually recover? What things should I avoid? In case I make matters worse, doctors will explain things.
Intro 10:54
But obviously, you’ve never had a stroke before, you probably don’t know what questions to ask. If this is you, you may be missing out on doing things that could help speed up your recovery. If you’re finding yourself in that situation, stop worrying, and head to recoveryafterstroke.com where you can download a guide that will help you it’s called a seven questions to ask your doctor about your stroke.
Intro 11:19
These seven questions are the ones Bill wished he’d asked when he was recovering from a stroke, they’ll not only help you better understand your condition, they’ll help you take a more active role in your recovery, head to the website. Now, recoveryafterstroke.com and download the guide. It’s free.
Bill Gasiamis 11:38
Well, nothing my first paid for my second bleed, then I would have been completely dissatisfied with the level of care that I was receiving. And 37 When my life’s on the line, I’m like, Well, I don’t think I’m going to cop this, you guys aren’t going to be that way while I’m around. And I’m going to do something about it.
Bill Gasiamis 11:57
And then I took responsibility for those things. Luckily, I was able to I was cognitively well enough just to be able to take responsibility for that stuff and to handle some of that stuff off to my wife. And, and we got through it. What bothers me about women who have taken them the the contraceptive pill, and they’ve been on my podcast, is that one of them, ask them? Did the doctors say it was the pill that did it. They do the hall while it may have been the pill that did it.
Jenn Williams 12:33
Yeah, they won’t cop to that.
Bill Gasiamis 12:36
Yeah, no one commits to it. It doesn’t say it on the box for no reason it says it on the box for a reason. And when you’re perfectly healthy, you don’t have any history for any of those conditions that cause blood clotting disorders. And you’re young, and you have a stroke, and you’re on that there should be a logical conclusion.
Bill Gasiamis 13:02
And this shouldn’t be this. We’re just going to wipe our hands from that, but I think that is the pharmaceutical industry, right? That is that whole, just give them this stuff. And you know, 99.9% out of the time, it won’t cause any harm, and it won’t cause any problems. And if it does, we’ll just deny it anyway, it will say it could have been something else.
Jenn Williams 13:25
Right? So they classify my stroke as cryptogenic. Because they’re not gonna say that it was officially the contraceptive. So they say that there’s no known cause. Well, if I don’t have any of the other risk factors, I don’t smoke, I take very good care of my body.
Jenn Williams 13:44
All of my numbers are good. Then what does that leave? But it’s like they’re too scared to say that. Which is really unfortunate because it leaves so much unanswered for people that are like myself, like you that are looking for answers.
Bill Gasiamis 14:02
And you’re looking to maintain your health as much as possible. Now that you’ve had a stroke, you want to make sure you don’t have another one. Did anyone say you should stop taking the contraceptive pill?
Jenn Williams 14:16
Oh, yeah, that was the first thing that the doctor said to me. Well, thank goodness.
Bill Gasiamis 14:20
Oh my gosh. So it probably wasn’t the contraceptive pill but stop taking it anyway.
Jenn Williams 14:25
Oh, yeah. Then the neurologist in the ER came to me and said you will never take contraceptives again. That was in the ER before I was even admitted to the ICU. Yeah.
Bill Gasiamis 14:40
I many years ago was coaching a lady who wasn’t on the contraceptive pill but she was on other medications. stuff again that she started in her teenage years for some conditions right for a particular condition.
Bill Gasiamis 14:54
And by the time I spoke to her, she might have been 2530 years into taking that particular medication. And the very first question I asked her was, is it still necessary for you to take that medical medication? Has that issue resolved? And she looked at me dumbfounded. She goes, I don’t know. I’ve never asked anybody. I just go and get the refill every, every however often, and I just take it again.
Jenn Williams 15:23
I just keep taking the medication.
Bill Gasiamis 15:26
And I was like, okay, cool. So the next time we spoke, she had spoken to her general practitioner, and they had begun the process to investigate her condition and her situation. And to determine whether or not it was a good opportunity to start removing herself from this particular medication stopped taking this medication.
Bill Gasiamis 15:50
And no one had followed up with her in all those years, and no one had said, How’s this going? How’s that going? In Australia, you have to go back and get a script, from your doctor, every so often, they’ll give you certain refills, and the pharmacist where you pick up the medication all day, every day, your entire life knows you by name by now, nobody kind of goes, what are you still don’t take in this, how are you going? Are you better? Have you recovered?
Jenn Williams – Self-advocacy For Medical Care

Jenn Williams 16:20
And I think I think that too, comes down to the piece of self advocacy, advocating understanding your body but also advocating for your body. And I’ve been very clear with my doctors, I don’t want to take on unnecessary things. How long have I been on this? Can I get off of this? And they know that that’s my stance. So I think being very clear and direct in that way can be really helpful. But like you said, a lot of people just don’t even think about it. They just, I gotta go get my meds and they take their meds and they go about their day, not thinking that they’re putting chemicals in their body and causing potential damage.
Bill Gasiamis 16:58
And disclaimer, neither Jen or I are saying, stop taking your medication. No, one’s saying that.
Jenn Williams 17:06
Good call Correct. No, one’s saying that or saying talk to your doctor.
Bill Gasiamis 17:11
Correct. And we are also saying that some medications are very necessary, and you have to keep taking them. And you must not be slug are taking them because they’re probably keeping your well and healthy. So there’s both sides of the spectrum. And we’re encouraging people just to know, just, yeah, where they’re at.
Jenn Williams 17:38
Just to ask, it’s and so I’m from Maine in the United States, and we’re the most northern state on the East Coast. And I do self advocacy training with support groups with a colleague from New Hampshire. And one of the things we tell people is, it’s your body, you have the right to ask questions about your body and about your care. That’s so important. It’s okay to ask a question. And so many people are too scared. It is okay to ask a question about your body. It’s yours.
Bill Gasiamis 18:13
I agree. I think maybe do you think maybe the recent pandemic challenges with medications might have thrown a bit of a spanner in the works, the way that they were suggested that they were taken, might have thrown a spanner in the works to comply.
Jenn Williams 18:34
In a way, I do think that there are some people that are and this is not a dig at anybody, but that there are more apt to comply than others. And for me, once again, I needed to do what was right for my body. And for me, I felt like we didn’t know enough yet. And I was not comfortable taking any vaccinations or anything like that. And I had a lot of people that were really mad at me, including my mother for making that decision for myself. And now looking back, I made the right decision. I don’t knock anybody for doing that. It’s just your own personal decision.
Bill Gasiamis 19:14
Same and on that point of the thing that you said I think which is the best you didn’t know enough. And you not only did you not know enough about that. But this is the point that’s the exact point. Most people don’t know enough about taking the contraceptive pill. Most people don’t know enough taking x y z and that’s the thing it’s that we don’t know enough, we haven’t asked enough, we haven’t learned enough, we don’t understand the ramifications, the complications, we don’t understand that.
Bill Gasiamis 19:43
I think we should understand it. Especially if the ramifications of not taking something as well and negative so blood pressure lowering medication, blood sugar lowering medication like if we are not doing other things As to support our blood pressure and our blood sugar. And we need medication.
Bill Gasiamis 20:05
We need to know the ramifications of the other side of the spectrum. What happens if you don’t like high blood pressure medication? stops people from having hemorrhagic strokes? And ischemic strokes? So we need to know more. And thank you for going on that tangent. That was a good one.
Jenn Williams 20:26
I think it comes with brain injury honestly.
Bill Gasiamis 20:30
It’s very relevant. Why don’t want to do that. I want to go back to before we went on that tangent, and I want to ask you about how did you end up leaving hospital with your family with you in the care of your family? And what kind of a decision was that that they made that they were going to take the responsibility for helping you get through this on? Like, how does that happen?
Jenn Williams 20:56
I mean, partly, I think it’s just that I’m just wildly independent, and so is my mother. And my mother is not going to accept me being coddled, I guess. It’s just not how I was raised. I was raised to be, you know, very independent and forthright. So I, they came in and they said, we really want you to go to inpatient rehab, it would be three to six weeks, you would have your daily PT, OT, those kinds of things.
Jenn Williams 21:31
And my mother was, no, because she’s seen family members go to inpatient rehab. And we said, okay, so what would outpatient look like, you’d be going to the outpatient facility three days a week, you would have your PT or OT, I did have a speech evaluation, which they just said, You’ll get better. And I didn’t have to go for speech therapy. But they really they kind of explained that the outpatient therapy was actually more intensive than inpatient therapy, because they have more tools in their outpatient centers than they do in inpatient.
Jenn Williams 22:11
So that was the other deciding factor was that when I first went to the neurologist, after my stroke, I didn’t understand. And I said, how long is this going to take? Like three months, I don’t have time for this. And now looking back, that outpatient decision was the right decision, because that was my attitude, going into it from the beginning, is I’m going to get better. I’m going to walk again and write again, and all of those other things, it’s not negotiable.
Jenn Williams 22:41
So how do I do that? That’s the most efficient way possible, which was outpatient. And I had an amazing experience with my outpatient rehab. And during the days, when I had appointments, my mother would come and take me. And then on the days where I didn’t have appointments, and my husband was at work, I had friends and family that would come and spend the day with me, because I was a fall risk.
Jenn Williams 23:04
So make sure that I, you know, could go to the bathroom. And that kind of thing. I wasn’t allowed to cook, because I couldn’t tell temperature in my hand. And of course, there’s all cognitive pieces to that as well. So I had friends and family that would come over and make me lunch and that kind of thing. And then in the evenings on the weekends, my husband was the caretaker.
Bill Gasiamis 23:28
That’s very cool. I get it now. That’s a great move. I thought that they took on your care. And I had no tools or sir or capabilities or skills to do any of that stuff. And I was fascinated to hear that story. But I think what you did was awesome, because I was in inpatient rehab for about a month. And I was I was like you I was maybe it wasn’t how long is this going to take but it was I’m going to put as much time and effort in as I can while I’m here to get a result. So I’d go home sooner.
Bill Gasiamis 24:05
And instead of being in for the two months that they had booked me in for was in for a month. And then I went to outpatient rehab and I had a similar kind of support structure where family would take me to and from. And my level of cooking was just low level of, you know, prepping a sandwich or something simple that didn’t require knives and standing for too long and all that type of thing.
Bill Gasiamis 24:36
And then family was bringing over food and then my wife when she wasn’t at work she was helping out and doing her her bit. So it was very similar. And I remember going to outpatient rehab, but I felt like it was a bit of a waste of time. I felt like I had done the majority of the recovery I got great results at in inpatient rehab. And then outpatient rehab, I ended up getting to the point where I said to the guys, I think I think I’m done with you guys, you’ve done a great job, and I’m gonna take the responsibility to improve my walking even more.
Bill Gasiamis 25:20
On my own, I’m going to do that at home, and I’m going to get better at home. But thanks for everything that you did. And one of the reasons I did that was because I was bothered. I had three appointments a week. And after about, say, nine months of best six months of outpatient rehab, that meant that I had to spend, and always around the middle of the day or something like that I had to spend half of the day, going to the appointment, doing the therapy, and then leaving the appointment and coming home.
Jenn Williams 25:59
And recovering from those appointments takes a lot out of you as well.
Bill Gasiamis 26:04
So it’s about three or four hours of the day that are gone. So I couldn’t be productive in other things. So it was kind of weighing up the all the pros and cons and then going, okay, the pros are that I’m really well, well enough to go home. And then I can definitely do more recovery on my own and save three or four hours, three days a week.
Jenn Williams 26:34
And I asked my physical therapist, I said, you know, how like, would you classify this injury as, because I call them a brain injury? would you classify this is like, mild, it doesn’t feel mild, because I’m learning to walk again, and learning to write again. And she said, I would call it moderate. And I said, I’m just trying to figure out if my recovery is because I’m younger, and I have more gray matter and I more easily leave covering, or if it’s because of like the type of stroke. And she said, Honestly, it’s because you show up.
Jenn Williams 27:12
And I said, What do you mean I show up? Of course, I show up. And she said the amount of people that don’t show up to their appointments is shocking. And when you miss an appointment, you miss a step in your recovery, just like you show up, you do the exercises, even if they scare you and make you uncomfortable, you still try them. And you you try and you show up and you do the work. And that’s what has made a difference in your recovery.
Bill Gasiamis 27:38
I would tend to agree with that. And even if it’s hard, you do it, even if it’s hard, and you do it even if you’re fatigued later. And even if you have to recover for half a day or a day.
Jenn Williams 27:51
And I cried in PT all the time. It’s just part of the process.
Bill Gasiamis 27:57
Yeah, you have to kind of push yourself, you’ve got to get beyond your limits. You got to find where your limits are. You’ve got to do everything. And it’s got to be you’ve got to be brave to just go places you’ve never been before emotionally, mentally, physically. Because you do get results, you get something back. Now, it might not be the same thing, everyone might not get the same thing back.
Bill Gasiamis 28:22
But you always get rewarded for putting in more effort when your effort is going towards trying to make you walk better use your hand better, balanced better, you’ll always get a reward by putting in more effort, especially when it’s supervised and you’re safe. And you’re in a good place. Why I like to think that people who are listening to this podcast or other podcasts that are related to health and wellness and recovery.
Bill Gasiamis 28:53
And overcoming challenges, and all that kind of stuff are always going to be better off than the people that are not looking for podcasts, to listen to, to learn from books, who are not asking to be on a podcast. It’s like, I don’t know what your condition is. I don’t know how bad you are. But if you’re on my podcast, or another person’s podcast, who talks about recovery and overcoming stuff, and how you’re beating the odds and all that sort of thing, you are likely to get a good outcome, you are likely to have an amazing life in 10 years from now.
Bill Gasiamis 29:27
And the people who aren’t I’m not saying if you’re listening, that’s not enough. No, that is enough. All I’m saying the people who aren’t considering any of that stuff, and are just feeling sorry for themselves. They are going backwards, they’re not going to achieve much.
Jenn Williams 29:46
And that’s another thing that I share in, you know, the trainings that I do is that part of my because people ask me, you know, how did you have such a great recovery? And one of the things I say is that I refuse to be a victim I’m not going to let this one medical trauma, destroy the rest of my life. I’m not going to sit back and say what was me and just be depressed for however many years I have left, too young for that that’s not acceptable to me. So I’m not going to be a victim. I’m not going to sit there and let life pass me by. And I think that that mindset makes a huge difference in recovery.
Bill Gasiamis 30:28
This this is saying that I’m gonna ruin right. And I’m gonna not say it right, for sure. It goes something like you fail 100% of the times you don’t try. So I’ve taken that to heart. It’s like, every time you’re afraid of something failing, because you tried it, and you weren’t good enough at it at the beginning. That’s not a failure. That’s a win every time you thought, I’m not going to do that in case I fail.
Jenn Williams 31:02
And you’re learning, you learn every time you fail at something.
Bill Gasiamis 31:08
So tell me a little bit about your background. What did you do for work? What were you doing to occupy your time before you had the stroke?
Jenn Williams 31:19
I was in banking for about 10 years. So I worked in commercial lending, I worked in the branch doing teller work, and I became a licensed insurance agent. A couple of months before my stroke, yeah. See, we I got my job in October of 2015. My husband and I bought a new house in January of 2016. I became a licensed insurance agent in May of 2016. And I had my stroke in August.
Jenn Williams 32:02
So I continued to try and go back to work. That was not not conducive. But I was I’m also a 31 consultant. So it’s direct sales. And there’s like bags and totes, and that kind of thing. So and I was a leader in that company. So I was working 40 or 50 hours a week as an insurance agent, about 15 or 20 hours a week at that job. And I was going to CrossFit three days a week.
Jenn Williams 32:31
I was actually continuing to try and go to CrossFit when my hand was tingling. And I was adjusting movements over that 10 days, because I couldn’t grasp correctly. But I mean, not that I don’t now but I had a very full life. It’s just a very different full life. Now I, you know, spent a lot of time with my family and made sure that I had a lot of fun things scheduled and to concerts and all that other stuff. I tried going to a concert, I think two or three years after my stroke, that was not a good idea.
Jenn Williams 33:08
I’m better now. But the sensory overload that Oh, my goodness. And that has been one of my biggest issues is overstimulation and sensory overload. Which I’m sure as you can understand, and I’m sure other people have said this on your podcast is that when people can’t see it, they don’t know it’s there. They don’t understand.
Jenn Williams 33:28
So they just say, Oh, you look great. You’re fine. But constitutively No. So I tried going to a concert, and it was not a good idea. I’m almost eight years post injury and I can do those now. But I’ve had to definitely adapt my life, it’s not what it used to be. It’s different. Does that answer your question?
Bill Gasiamis 33:52
It does. I wanted to get a sense of like, how you were and how you hang out now what you do now. I was the same. You know, work was no problem. I was 37 It was everything was happening fine. Tried to go back to the football which was the thing and people would invite me to go to the football I said I think I want to avoid that I don’t want to go there’s too much noise and yelling and cheering and bright lights for a night game and all that kind of stuff. And it was really difficult to be there.
Bill Gasiamis 34:24
Tried to go to a couple of venues where family would have a party or something like that or get together and then that would be an early night a lot of the times you’d be I think I’ve had enough at around 930 or 10 o’clock and it’s this go home and then I did go to an AC DC concert with my sons and here in Melbourne and I went with ear protection so that it can dial the right sound a little bit and I could still be there because of my Favorite band.
Bill Gasiamis 34:57
And then I still will avoid loud rooms, if I can noises, TVs and all that kind of stuff. Everything’s always on, you know, as low as possible. And even these lights that I have next to me and, and in front of me on the podcast where I where I record, even they bugged me. They’re on for an hour. And they bugged me. But like, yeah, you need, you need some lighting, so I can put up with it for now. So it’s okay. So what deficits do you have now? How does the body feel now?
Post Thalamic Stroke Recovery And Deficits
Jenn Williams 35:36
I’m mean, overall, I’ve had a really good recovery, I still have my struggles. But I’m really grateful for the recovery I’ve had, I still have some balance issues. I started going to yoga and bar. I don’t know if you know what Barr is. It’s like a combination of like ballet, yoga and strength training. So it really focuses on those little muscles, which I realized is what I needed to focus on to help my balance. So that’s been helping very slowly, but it’s a very, very slow process. So balance is still an issue, and insomnia.
Jenn Williams 36:18
I have terrible insomnia. It’s really bad. I’ve been working with a naturopath to try and get that fixed because I was not getting answers in the standard medical world. And then cognitive, really, that overstimulation? I call it delayed memory, like I will remember things a couple of days later, which I had a neuro psych evaluation. And they said that that’s actually stroke onset ADHD, I didn’t know that was a thing. So it can’t be treated with medication because it’s due to brain damage. So I just kind of have to navigate as best that I can with all of that.
Bill Gasiamis 37:04
And stroke onset ADHD makes you remember things two days down the track.
Jenn Williams 37:11
So it’s because if I’m not in a focused environment, like right now, if you and I are talking, and you know, my husband comes in and says, you know, hey, can you do this when you’re done? I won’t remember that. If he says, Hey, I need your attention. And they says, Can you do this? Yes, I can. But it’s because of that distraction, that ADHD that I had my testing done, and they said, my storage and recall is fine. It’s just that there’s this delay in me finding the information that I have stored in my brain.
Jenn Williams 37:44
And it’s because of distraction. So that’s been an adjustment, I’m trying to use post it notes and alarms on my phone, and calendars. And I have the calendar on my phone, and I have a paper calendar. And then I have a family calendar, and I have all of those things to make sure that things don’t fall through the cracks, cracks, they still do sometimes. But that’s been an adjustment, as well.
Jenn Williams 38:12
And then that overstimulation piece like I mentioned, the hardest thing for me has been the grocery store and driving. Those are very complex tasks for the brain, and you don’t realize it until your brain is misfiring essentially. So I’ve worked really hard to get to the point where I can do those things. I don’t know if you guys have this in Australia, but there’s a company in the United States that does music therapy for cognitive health.
Jenn Williams 38:43
And I use them which made a huge difference. And I went from not being able to drive for more than maybe 15 minutes to driving an hour, hour and a half. And like going having lunch with my friend and driving back in an hour. So that made a really significant difference in my recovery. But when I’m tired that all flares back up.
Bill Gasiamis 39:06
And then the brakes get put on I know that I know that when I’m tired thing the wall comes up from out of nowhere.
Jenn Williams 39:15
That’s a great description a great analogy “The Wall” it’s exactly what it is.
Bill Gasiamis 39:20
That’s what it is. And it’s like I’m here again. All right. Okay, I’ll stop I’ll sit down and won’t do anything now for the next however many hours and for me the wall’s getting shorter and shorter. But it still pops up it still kind of says you’ve done too much. You haven’t rested enough you didn’t have a good night’s sleep. Time to sit down and do nothing. And that’s it and everything just sort of shuts down like you say like in the movies. You know when a button is switched off on the robot and everything just goes.
Jenn Williams 39:56
Powering down.
Bill Gasiamis 40:02
That’s exactly it. So, man, I was gonna ask you a question about something you just said about your Oh, yeah. Music therapy. So what’s that based around? Is it based a certain frequency range that you listen to? How does that work because I have used, and we do have people who offer music therapy.
Bill Gasiamis 40:29
I’ve never gone to a music therapy session, but I have listened to certain meditations that are at certain frequencies, to get certain waves, beta waves, theta waves, all that kind of stuff going, depending on what you want to achieve. So tell me about what you did.
Jenn Williams 40:47
So this is what I experienced is different than that. But I do use those meditations, like you mentioned, especially delta waves for sleep, so I use those. But this music therapy was to help me with my divided attention, the stroke onset ADHD. And basically, what the therapist would do is she would have a guitar.
Jenn Williams 41:08
And then she would have a drum playing on her computer. And she would say, random letters, and I had to raise my hand whenever I heard an H, but only if the drums were playing. So I had to listen to her guitar, listen to the letter, listen to the drums, and then make a decision and acknowledge it physically with my hand.
Jenn Williams 41:32
Our pool is very complex, but their intake, you know, they do an intake and you know, our exam, just like any other provider, my intake, I was at, like 67% accuracy. And when I left, I was over 90%. So there’s proof in those that that made a difference, for me a significant difference. So there was a lot of different things like that, or she would tell me, she would play notes.
Jenn Williams 42:02
And I had to tell her, basically, whether they were the notes were going up or down from the previous one. So I have to listen and kind of process the two different tones. Was that first tone lower? Or is the second tone lower? So that required some additional divided attention as well. So it was really it was really interesting.
Bill Gasiamis 42:27
Did you also learn you weren’t tone deaf?
Jenn Williams 42:30
Yeah, I used to play music and in school and like high school, so I know I’m not tone deaf. Not completely anyways.
Bill Gasiamis 42:44
Good. I’m glad you got that.
Jenn Williams 42:46
I did I like it.
Bill Gasiamis 42:50
That’s cool. He’s mentioned earlier a little bit about advocacy work that you do about that? What do you do? Who do you hang out with? What? What spaces do you do that in?
Jenn Williams – The Middle People Project
Jenn Williams 43:02
So I’ve done some speaking at some support groups, I’ve done some speaking to college classes for future like speech language pathologists, to kind of talk about brain injury and how they can actually make a difference in brain injury or recovery. I can I plug I don’t want to like plug a business or anything.
Jenn Williams 43:30
But I want to tell you about this project. So I told you I was teaching self advocacy with a colleague from New Hampshire. So I also am on the advisory board for the Brain Injury Association of America, Maine chapter. So they look for survivor’s input. And I also did some administrative support for our legislative council that deals with brain injury law.
Jenn Williams 43:58
And in all of those meetings, I have said, what about the people in the middle? Because they talk a lot about these, you know, government waivers and Medicare and you know, how many spots we have and who’s getting services and all this other stuff? Well, those are very small numbers.
Jenn Williams 44:18
So what about the people in the middle? What about the people like me, that didn’t go to inpatient rehab, I went home, I did outpatient for a year. And I’ve been trying to figure it out on my own for eight years now. I stuffed the primary group that I see at support groups these people that aren’t eligible for certain services, either because they’re “not disabled enough”, which I’ve been told, or they don’t meet qualifications financially.
Jenn Williams 44:50
So they’re just left to not much for resources. So I shared this idea over and over again, wasn’t really welfare saved. And then I shared it with my colleague from New Hampshire, John, and he shared it with his colleague, David. And David took it and ran with it. He was like, this is an amazing idea. There’s millions of middle people if you actually break down the numbers.
Jenn Williams 45:15
So the three of us have started The Middle People Project. So we’re trying to create a hub of resources for people that feel like they’re in the middle. They don’t qualify for services, but they feel like they still need help. And they’re not as fully recovered as they’d like to be. I don’t think anyone ever fully recovers. So I don’t like to use that term.
Jenn Williams 45:36
So we’re trying to offer self management strategies, and eventually do you know, a blog and helpful resources, that kind of thing, because there’s so many people that just need a little extra support, and they don’t know where to go. So that’s another kind of passion project that I’ve been working on in the brain injury world, I have all sorts of ideas. So we’ll see where, you know, next year, I could be on a totally different project. I don’t know.
Bill Gasiamis 46:07
Yeah, well, if you’re ADHD brain has anything to do with it, you definitely will be.
Jenn Williams 46:12
Oh, it does. That’s why I have notebooks everywhere.
Bill Gasiamis 46:19
Yeah, that’s really cool. So I was one of those people stuck in the middle, I received some health care, and some rehabilitation, got a really good result was happy, didn’t feel like the job was done, and then wanted to do more. And then continuing to do more, I consider myself fully recovered, but not from the damage that was done, the damage is there, and my deficits are there. But if I call myself fully recovered, it’s probably from the emotional side of that. And the mental side of it. Although I did my book launch about a week and a half ago.
Jenn Williams 47:00
Congratulations.
Bill Gasiamis 47:02
Thank you, thank you. I was in tears. So often in my presentation in my speech, and I had to start making jokes about it. And during the presentation, it was so there was so much of it. And I didn’t realize I was going to have such an outpouring of emotions in that way that it was going to be so evident. And I had to catch myself a few times. But the good thing about being emotional in front of people is, as soon as you cry, you’ve got them hooked. So it didn’t matter, every time I thought I was losing them, I just chucked a few tears out there and just bring them back again.
Jenn Williams 47:02
Yeah. So I applied to speak, to share my survivor story at the main brain injury conference this fall. And because of all my work, I know quite a few people at the Brain Injury Association, and one is my friend Sarah. And I would say it was like two weeks after I applied. I had a really long day at my job that I have now, which is working at a property management company. And I overdid it. And I realized that I was at the office and I couldn’t drive home.
Jenn Williams 48:20
So I ended up laying on the floor for like a half hour until I felt safe to drive home. And I’m on my way home, just sobbing. And I call her and I’m like, who am I need to talk about recovery and mindset, if I am sobbing in my car, eight years later, and I overdid it. And she’s like, that’s why that’s literally why because that’s relatable because survivors deal with that every day. And I just had this moment of like, I don’t have this under control at all. I thought I did, but I don’t.
Bill Gasiamis 49:03
Exactly. I’m 12 years out and here I am speaking in front of a whole bunch of people who came to see me talk about a book, you know, and I think that just goes to show that that’s, you know, that’s just human that’s just being human that’s that’s all that is, not anything else. And it’s good to be able to share your express your emotions, to have the understanding as well, that I need to lie down, I can’t drive and rest.
Bill Gasiamis 49:31
I often would find myself jiving many years after the brain surgery and kind of get the whole nods happening you know, oh my gosh, don’t think I’m I’m fading. All over Find a quiet spot under a tree had just sleep. Sit down, say for 2030 minutes as long as I needed. And then I would start the car and go again.
Bill Gasiamis 49:59
And it was necessary, without it, I definitely would not have made it home safely. And it was simply because of that overwhelm of perhaps the distance I traveled, the amount of time I was concentrating cars going by whether it was raining, or whether it was sunny, everything impacted, the way that I would experience that drive and everyday was different.
Jenn Williams 50:27
Driving is a very complex thing for the brain, there’s a lot of input that’s happening, you’re looking at the road in front of you, you’re looking at the road to the left or the right, depending on what country you’re in, you’re looking at the other lanes watching the traffic, you’re looking on the side of the road for any potential hazards, you’re looking in your rear view and your side mirrors.
Jenn Williams 50:48
And for me, the biggest issue that I was dealing with was the shadows from the trees, at certain times of day, they would create like a strobe effect. So it felt like a strobe light while I was trying to focus on all of those things. And similarly, like you said, if it’s raining, raining with the windshield wipers, it would feel like a strobe going in front of my eyes. So it just you don’t realize how complex it is until your brain is trying to basically learn it all over again.
Bill Gasiamis 51:20
Yeah, that’s that’s a legitimate reason to feel like you need to lie down and restaurant you have to it’s yes, it’s necessary. 100%. And I’m like you like it does make me doubt my qualification of being a podcaster promoting all this stuff. And, you know, being an advocate and all that something kind of does make me question my qualification.
Pain Management And Personal Growth
Bill Gasiamis 51:47
And makes me do silly things like, it makes me have like, imposter syndrome every once in a while still. And all that type of stuff. It’s crazy. I still get that even though I’ve done more than 300 podcast episodes, I’ve written a book, I still feel like a bit of an impostor, because I kept remembering the person that I was before stroke. And I was, and I wasn’t not this kind of guy. Like I didn’t do anything public. You know, I wasn’t out there. And I still feel like my identity hasn’t caught up with all the stuff that I’m making it do, that it hasn’t signed up for.
Jenn Williams 52:33
Yep, I absolutely understand that.
Bill Gasiamis 52:37
And I don’t even know why I’m doing it all sometimes, why the hell am I doing? Why am I doing my 300 and 10th podcast episode that’s like.
Jenn Williams 52:48
I can tell you why. Okay, number one, it’s fulfilling to help other people, just in general. Number two, there is such a lack of voices and information around brain injury. So you’re making an impact by spreading information. And number three, it’s healing to connect with other people that have gone through what you’ve been through,
Bill Gasiamis 53:11
Tick, tick, tick. That’s exactly why.
Jenn Williams 53:18
Because I do the same thing I’m always looking for, like, how can I make an impact? How can I, you know, help this person? What resource do they need? That’s my same drivers as well.
Bill Gasiamis 53:31
And sometimes I feel incapable of actually helping and making an impact. And because a friend of mines daughter had a hemorrhagic stroke last year, and she was 17, at the time, I was in ICU with him. And you know, we struggled together. They’ve come a long way, and she’s a lot better, but she’s got pain now in her left foot.
Bill Gasiamis 53:58
So when things started to settle down, the numbness turned to pain and the pain kicked in. And she’s struggling.
Jenn Williams 54:09
How long ago was it?
Bill Gasiamis 54:13
It was in the last 12 months. And now she’s struggling dramatic pain, because of where the stroke happened was the area of her brain where pain receptors do that work, right? That’s as much as I know about it.
Jenn Williams 54:29
Was it the thalamus?
Bill Gasiamis 54:32
It was in the middle of the brain near the very center of the brain. Right side, when you see the brain scans, you see the two sides of the walnut and then in the middle, there’s kind of like a bit of a gap. The bleed was from the right side, she had an AVM that damaged the right side, but it bled into that gap between the two pieces of the walnut.
Bill Gasiamis 55:01
Anyhow, they drained it and she’s got an amazing result, right. But she’s got this pain now. And that’s the thing. It’s like for me, I realized the works not done. And I don’t know how I don’t know how useful it is this podcast to people who haven’t had who have pain who feel debilitating pain.
Bill Gasiamis 55:23
And I can’t relate to it because I didn’t feel that I feel a little bit of pain, but not ridiculous. She’s not able to sleep because of it, and it’s causing some drama, so that I feel I still feel like I’m not doing enough, like, my work is inadequate.
Jenn Williams 55:40
Because every injury is different. I used to hate that phrase, that every brain injury is different. But I’ve learned to accept it and actually appreciate it. Because that means that you’re not pigeon holed into one recovery timeline, or whatever it may be. So even though you might not relate to her on the pain level, the general concept, you know, is all very similar.
Bill Gasiamis 56:16
And I’ve seen that other side of what stroke does to families, because she’s got great parents, and they’re doing a good job, and it’s all good. But I can see the strain on the family, and the mom and dad and what they are going through. And then I just think about that. So it’s on my mind a lot more.
Bill Gasiamis 56:39
And I’m getting a little bit overwhelmed by it, not in the it’s not going to shut me down or stop me from doing what I’m doing or anything. But you know what, my heart goes out to them. And that’s what it is. And I just don’t want them to be in that situation. And I hope that they have a result a resolution and they’re going after every possible resolution, you know.
Bill Gasiamis 57:01
So, yeah, it’s just man and this guy, this guy I grew up with. I’ve known him since I was about four years old. And he is a radiographer, I wrote about him a little bit in the, in the acknowledgments in the back of the book. And he helped me out with all the brain scans that I did so he and his team would be taking my brain scans at the hospital that I was at, at the Royal Melbourne Hospital.
Bill Gasiamis 57:31
And he wasn’t meant to, but he would come after the scan and go, it’s looking alright, or because I was I had about eight or nine MRIs in the time that they were monitoring the blood vessel that burst the AVM and he would come and go, it doesn’t look like it’s changed, things have settled down a little bit, etc.
Bill Gasiamis 57:52
And stopped me from waiting about one month to get the news with my doctor. So that was really cool. And then to be in the damn hospital ICU with his daughter on life support because of this same issue that I had 11 years later, it’s just crazy. I just can’t comprehend it. But it was great to be that guy that was able to walk in the ICU and show them what is possible. Without saying anything. All I had to do was walk in there.
Jenn Williams 58:38
Can I ask you a question? Have you seen any gains or changes as you’ve gotten farther away from your injury?
Bill Gasiamis 58:52
Yep. Cognitively, things are improving still. And physically things are stable to slightly declining. But the decline is not something that I can address. So what I noticed is my balance gets worse sometimes. And my pain and the tightness and the spasticity in my left side gets a little bit worse. Now again, nobody would know.
Bill Gasiamis 59:31
If I said that to somebody that knew what spasticity looked like. For some stroke survivors. That would go you don’t have spasticity. But the feeling that I have has sometimes, sometimes gets worse. And recently I kind of smiled when I said recently I fell off a ladder. And the reason When I fell off the ladder was because my left hand gave away it just let go of the ladder. And that does happen from time to time. And usually it lets go of a bottle that I’m holding or my telephone.
Jenn Williams 1:00:12
I had that happened with my purse last week. I was really tired, I was holding my purse and my hand just let go.
Bill Gasiamis 1:00:22
Yep. I’ve lost the phone because of that. All sorts of things. But then this time, I was climbing a ladder, I was only two rungs up, I was going up to the third rung. And my left hand just let go.
Jenn Williams 1:00:39
Thank goodness, you weren’t further up?
Bill Gasiamis 1:00:41
Well, I still fell backwards. And I fell onto a middle bar, a scaffold bar. Because my full time business is we have a property maintenance company. And in order to do the repairs on this particular home, that we’re working on, I got a scaffold so we could be safe.
Jenn Williams 1:01:06
The irony.
Bill Gasiamis 1:01:07
Yeah. So I’ve fallen off the ladder backwards onto one of the horizontal scaffold bars that are holding the construction of the, you know, all the poles together, it broke my fall, I landed on my ribs. And then and then I fell another three feet, or a meter to the deck below and hit my head. So it was quite a shock to find myself down there. And then I couldn’t sleep properly for about a week. And then I started to sleep better after that.
Bill Gasiamis 1:01:43
And it’s been around three weeks, and only for the first time last night, I was able to lay on my side, haven’t been able to do that for three weeks. Because of the pain, I got it checked out. There was a lot of bruising, there was no broken bones or anything. But that is not an escalation of my condition. It’s kind of what my condition is doing.
Bill Gasiamis 1:02:07
And I think what it’s doing is it needs more TLC, it needs more therapy and more rehabilitation, I’ve been going to the gym trying to strengthen my left side. And I still, you know, eat well, and all those things, try and get as much sleep as I can. But I think my left side is becoming more needy, and I’m not putting enough effort in. And it feels a little bit number.
Bill Gasiamis 1:02:41
And maybe, and in winter, it always gets worse. It’s getting into the winter months now. We’re first day of winter today here for us. June the first and and I think in winter, my sensation decreases on my left side, it gets more colder and more numb. And I remember now that you asked me thanks for asking this because it’s just reminded me everything my mum,
Bill Gasiamis 1:03:06
I was at my mom’s the other day. And I was in her way. And she was just trying to not interrupt my conversation and kind of squeezed through him. But I wasn’t paying attention I didn’t notice. So she went to pinch me on my bum. And she said, Why aren’t you moving out of the way? And why aren’t you responding? I said to what? Because I’m pinching you on the bum. I can’t feel it. She says really? She thought I was joking, and that I was just putting up with it. I couldn’t feel it at all. I had no idea she was doing it. So yeah, those types of things are happening now.
Jenn Williams 1:03:48
Have you heard of something called post stroke? recrudescence? No, do tell this is my favorite topic. You’re gonna love it. Um, so there’s been there was a study done at Massachusetts General in I believe it was 2016 or 2017. And then the American National Institutes of Health just did a study on it, I believe last year.
Jenn Williams 1:04:14
So the basic explanation how this was explained to me is that when you have a brain injury, and you have neurons that die, the neurons around the dead ones, eventually pick up the job of the dead your neurons as their second job. Well, if your body feels like there’s a crisis, which in the body or crisis can be that you’re tired that you’re stressed. It could be you have low blood sugar, the brain can say, oh crisis, we need to focus on our first job and it stops doing the second job.
Jenn Williams 1:04:53
So I have symptoms that flare up. When I’m really stressed when I haven’t slept At if my I didn’t really have blood pressure or blood sugar issues, but you know, things like that that could be considered a crisis in the body. And my brain goes, Nope, we’re not doing those things. So my hand stops working, I get tingling in my hand tingling in my face tingling in my foot, my balance goes, I get vertigo, all these other symptoms, and it can feel like another stroke or it can feel like just after my stroke.
Jenn Williams 1:05:28
So I’ve gone to the ER before, just to make sure I get checked to make sure that something else isn’t happening. And I’m usually fine. But I learned about that. And it made so much sense. And when I talked to other survivors about it, they go, oh, yeah, when I’m tired, all my symptoms crop up. When I’m really stressed about dealing with my doctors, all these symptoms pop back up. So it might not be necessarily decline. It could just be you’re not at homeostasis, for lack of a better word.
Bill Gasiamis 1:06:03
I love that explanation. I think that’s also is valid. What you just said is definitely valid. Classic example is if I have an argument with my wife. Happily married for 19 or 20 years. So I get more symptoms. Yes. So when that I’m in emotional, negative emotional state, I get more symptoms. And it encourages me not to be there for too long. And I’m getting better at not staying angry or mad for ever, and ever. So there’s that. I agree with that. That does happen. And I’ve said it a few times on the podcast. And when I eat the wrong food.
Bill Gasiamis 1:06:56
For me it’s like, say a pastor, or a sugary drink or something like that. Oh, my gosh, things just get so much worse. Brain fatigue, fog, tingling, balance, everything kind of just gets worse. So I agree with what you’re saying. I may have. And that’s a thing, because it’s happened recently a number of things have happened that have bugged me that have made me think but going to the mind goes to maybe it’s getting worse.
Bill Gasiamis 1:07:26
I don’t know that it is I’m not It’s not stopping me from doing anything. Although I am very cautious about letters. Always have been even though I fell from one, I always have been. Yep. And what it says to me is I just need to go and get more rehab, more therapy. That’s all it says. And I’ve been at massless chiropractors, this guy that I’ve been there the whole time. And they know me really well. So yeah, I don’t know. It’s always changing. And I’m always adjusting. And I’m always finding a way, a way to overcome it.
Jenn Williams 1:08:09
I do think that learning about the poststroke recrudescence helped me to be more self aware. Because when I have those symptoms flare up, I can take a step back and go okay, what does my body need right now? Did I get my electrolytes today? Did I take my medications? Maybe I forgot my medications. You know, maybe I forgot my aspirin or you know, whatever. How did I sleep last night? Am I stressed? Do I need to go move my body like so it gives me that pause to kind of have a little self evaluation to see where I’m at.
Thalamic Stroke Recovery: Insomnia Causes And Solutions
Bill Gasiamis 1:08:50
Yep, I love it. I agree with that. That’s what I do every time I hit a wall, that wall is just the just have a wrist wall? Or is this the do something more than wrist wall? Like what is it? What do you have to respond to? So yeah, for me for work, because I’ve got a couple of guys working with me, I’ve got a business partner. I could just say, I’m not coming in. I need not to be there. And then I won’t be there. That’s been a good thing that I’ve been able to do. Of late. Tell me about your insomnia a little bit. So is it insomnia that had begun after all your medical issues? So what’s it like? How did it begin? Can you describe it? Explain it?
Jenn Williams 1:09:40
Well, you know, when you talk about insomnia with your doctor, they’ll ask you is it that you have trouble falling asleep or you have trouble staying asleep? For me, it’s both I have trouble falling asleep and staying asleep. And I actually didn’t realize I guess that it was insomnia at first but cuz I was so fatigued all the time, I just figured that I was just fatigued.
Jenn Williams 1:10:05
And I was talking to my counselor, and I can’t remember what did I say? I said, I said, I can’t get out of bed. I’m exhausted, and I’m so frustrated. I must be depressed, blah, blah, blah. And he said, Well, depressed people aren’t frustrated about it. So that’s probably not it. I said, Oh, okay. And he said, How have you been sleeping? And I went, Oh, not well, no.
Jenn Williams 1:10:35
And I push, I learned this probably a year or two after my injury. And I was trying to take care of it on my own and trying to take melatonin and trying to just adjust my life around my sleep schedule, and all these other things, and it wasn’t working. So I eventually got a in lab sleep study in Boston. And they said, Yeah, you have sleep latency, your cycle has shifted. So you just need to adjust your life around your new circadian rhythm.
Jenn Williams 1:11:14
Well, that’s semi practical, that’s not extremely practical. So I talked to my primary care and gave me some prescriptions and tried a bunch of different ones. And I eventually started seeing my naturopath for something else. And we got that addressed. And she said, Is there anything else you want me to help you with? I said, Well, if you could figure out my sleep, that’d be great.
Jenn Williams 1:11:43
And she said, Sure, we did some adrenal testing. And it turns out that I was making melatonin at the wrong times a day. And I had like, no cortisol. And then I found out, yeah, for those of you that don’t know, a lot of people think that cortisol is the stress hormone, but it’s actually the counterpart to melatonin. So it’s what wakes you up in the morning, it’s what keeps you going through the day.
Bill Gasiamis 1:12:05
So the too much cortisol can be stressful. Yes, cortisol is necessary, because it’s, it’s the wake up hormone, it’s the wake up part of the sleep cycle, the thing about it is is, once it kicks in, you want to see it drop off, after it’s got you awake, you want to say drop off, and then at the end of the day, when the sun starts coming down, you want to say cortisol, not be there. So that right, melatonin, can start doing its job of putting your body into the sleep cycle.
Jenn Williams 1:12:42
So I was I had very little to almost no cortisol in the morning, your cortisol levels supposed to be like at a 25. And I was at a three. And then the afternoon, you’re supposed to be between like a five and a 10. And I was point five. And I was also getting a melatonin spike in the afternoon. So my melatonin would jump really, really high at like three o’clock in the afternoon.
Jenn Williams 1:13:07
So my hormones were all messed up. Another side note, I realized through doing my own research through all of this, that more than half of brain injury survivors have some sort of adrenal dysfunction, which is where your cortisol and your melatonin is produced. So we did this adrenal test, found this out. And I’ve been using different medications to kind of retrain my adrenals.
Jenn Williams 1:13:37
I used to sleep until noon. And now I get up at like 830. And that has taken me a couple years to force yourself to retrain and like get up at seven o’clock in the morning and take my cortisol so that it produces at the right time. Ah, yeah, I don’t have to take it anymore. My body has figured out the cortisol part. So now I’m working on the melatonin part. But I feel so much better.
Jenn Williams 1:14:07
Even though my sleep is still very broken. I sleep for like three hours, I’m up for a little bit and I sleep for three hours. But I’m getting more restful sleep, and I have that natural waking cycle that’s supposed to happen. So it’s been a very long journey. On the insomnia piece.
Jenn Williams 1:14:26
I’ve done all of the healthy sleep habits, no technology, two hours before bed, listening to delta waves, meditating, reading, you know, dim lighting, essential oils, all these things to try and create this like almost romantic sleep situation. And it really was just my adrenals that needed to be retrained. So it’s been a very long process but it is worth it.
Bill Gasiamis 1:14:53
I love it because you have got a positive outcome and that just goes to show you it is something that you can address And it’s whether they’re looking Yes, deeply enough into it. When I typed in cortisol deficiency into Google, it says, cortisol deficiency occurs when the adrenal glands do not produce enough cortisol, this can happen for four main reasons when the pituitary gland is unable to produce the chemicals needed to tell the adrenal glands to switch on the cortisol production. So it’s, it’s a proper brain communication signaling issues. So what I why I read that was if anyone’s struggling with this sleep is to ask the big questions beyond kind of have a sleep medication.
Jenn Williams 1:15:48
I didn’t want to be on sleep medication. I didn’t want to be on that crazy stuff for years and years. I wanted to fix it. And you know, instead of just saying, I don’t know, I don’t sleep well. Give your doctor details. Explain, I’m not falling asleep while I’m waking up every 30 minutes, because that’s what I was experiencing, I was waking up every 30 minutes, and I would be up for an hour, hour and a half. And it was like naps, all day naps, because I was still out of balance. So asking the very detailed questions and being very open about what you’re experiencing can really make a difference.
Bill Gasiamis 1:16:28
Get your pituitary gland checked out, get your adrenal glands checked out, get your thyroid checked out. Don’t just leave it at an some medications sleep because I’m not sleeping properly.
Jenn Williams 1:16:44
And I had a thalamic stroke, which I have since learned, because I did not know this that the thalamus is the distribution center of the brain. So all of the information that comes in, goes through the thalamus and then gets sent out. So when you have damage to your Thalamus, it can affect everything. Because the thalamus communicates with everything. So it could depend not even your pituitary. It could be the lambic issue, it could be any number of things.
The Hardest Thing About Stroke For Jenn Williams

Bill Gasiamis 1:17:15
Yeah, yeah, it’s important to know where the stroke happened and what part of the brain is impacted. And what that part is, does for a living, you know, how it pays its rent. So that’s awesome. I’m glad you’re getting a result and you’re seeing an improvement. As we come to wrap it up, tell me a little bit about what the hardest thing about stroke for you was?
Jenn Williams 1:17:42
Ah, I would say grief, the grieving the loss of my old life. And my old identity, I realized that I had really begun to absorb a strong, deep work ethic as my identity. So when I couldn’t work, I didn’t know who I was. I was like, I don’t, I am not working 80 hours a week, and busy and all those other things like I don’t know myself. And I had to grieve the loss of that old life.
Jenn Williams 1:18:22
And I still have days where I cry, and unlike what happened in my old life. And you know, the the loss of some relationships, there are, you know, you were talking about the family thing earlier, my family’s wonderful, but I do have some family members that have never really asked me about my brain injury that have never shown any curiosity and how I’m doing which is eye opening.
Jenn Williams 1:18:56
And then I have friends that just couldn’t handle it, they just could not handle the fact that I was on this road to recovery. And, you know, wasn’t just accessible to them 24 hours a day or anything like that. So I think just in general grief is a is a really huge part of it. And I think that’s the hardest part for me was the grief.
Bill Gasiamis 1:19:20
The loss of identity is very interesting one I speak about that in my book as well. I think it’s chapter three. And the good part about that is you can rehabilitate your identity really quickly. Yes, that’s a good part about it. You can become involved in all those things that you’re become involved in to keep you busy for another 80 hours a week, but just in a different way. And you pick up relationships in those new spaces, just like you were interacting with people in those old spaces. So that’s really cool.
Bill Gasiamis 1:19:59
The friends one is an interesting one, because many stroke survivors experienced the same thing. It says more about the people who kind of step away or don’t know how to handle it than it does about you. And I think it’s a blessing that they move away and step away.
Bill Gasiamis 1:20:23
Because if they’re incapable of supporting you, or being okay, or normal, or just be there, they’re incapable of doing that, then I think that would make your recovery harder, it would cause some stress or some aggravation, or whatever. And I think they do a really good job of going. I don’t know what the hell I’m doing here. I’m out of it. I’m gone. It seems weird, and it seems like a bit of a letdown and that they’re not doing what you would expect of them. But I think they’re doing the best thing they could possibly do. And that’s like, go away.
Jenn Williams 1:21:02
I mean, if that if that would be hard for them, then I don’t want them to be present. That’s not fair to either of us. I do also want to just talk a little bit about gratitude. I, my counselor asked me one day, he kind of said, Oh, I bet if you could go back in time and change it, you would. I thought about it. And I said, No, actually, I wouldn’t. And he said, Okay, you got to explain that to me. And I said, I have met people that I never would have met. Without being on this journey. I’ve connected with people.
Jenn Williams 1:21:47
And it changed me for the better. I have more internal peace. I don’t feel the need to push myself to work 80 hours a week anymore. I’m happier. I appreciate so many little things. Every day, I write down three things that I’m grateful for. And sometimes I’m grateful that I have really nice sheets on my bed. That’s okay. And I never would have had that much gratitude prior to my injury.
Bill Gasiamis 1:22:19
I relate to that. That’s why I wrote a book called The Unexpected Way That A Stroke Became The Best Thing That Happened. And people think I’m mad.
Jenn Williams 1:22:25
I know. I saw your title. And I was like, yes.
Bill Gasiamis 1:22:32
People think I’m mad. And it’s like, I’m not saying anything positive. Although there is positive things. I’m not saying that pain is good. And all this is like, we should suffer indefinitely. And it’s suffering is amazing. With a purpose it’s okay. It’s manageable. Yeah. Suffering, and then you convert it into a purpose, like a podcast, or helping other people at a homeless shelter or whatever. Like it transforms. I can’t explain how, but it just does.
Bill Gasiamis 1:23:07
And it makes it less shit. And then that’s all I want. I want it to be less shit than it was yesterday. And if it is, then that’s okay. And yeah, it’s like, I don’t know, I would love to learn the lessons without going through stroke. But it didn’t happen that way. I wasn’t that wise, I wasn’t that intelligent.
Jenn Williams 1:23:36
We apparently had to get some knocks in the head to get the point across.
Bill Gasiamis 1:23:42
A bit thick in the head. So it’s something needed to change, maybe a bolt of lightning or something or jolt or something. It’s just intensely crazy that you would say that that you would say I wouldn’t change it. I have met so many people that wouldn’t change. What happened to them? It’s just crazy. And it’s counterintuitive. What is something that stroke taught you? Did I already ask that?
Jenn Williams 1:24:19
I don’t think so. If you did, I forgot and we’ll say it again. Ah, gosh, something that stroke has taught me? It has taught me so much. I guess it’s hard to pinpoint one thing. I would say probably the gratitude piece obviously that’s a big part and then the it’s okay to advocate for yourself. It’s okay to ask questions about your health care. And I say It’s all the time and some people don’t like it, but your doctors or your employees, you can fire them.
Jenn Williams 1:25:05
If it’s not working, it is not working, and you can move on to the next. And that has been a huge change for me to say, You know what, this isn’t a good relationship, I’m moving on to the next person. And just having the self awareness and the comfort in saying that brings a whole new depth to self-advocacy for me internally, in all aspects of my life, it has taught me to stand up for myself in critical moments that I really need to.
Bill Gasiamis 1:25:41
That’s profound. It’s so good to stand up for yourself, and to take them on, and to just make them accountable. That’s all. That’s all you’re doing. Just checking out the information they’ve given you is accurate, and it’s applicable to you. And it’s the right information. It’s no different to what they do to you, when you get asked by 25 different health professionals in the hospital. What happened to you? So what happened to you? It’s on the chart, read the chart, but tell me what happened to you.
Jenn Williams 1:26:17
I told your nurse, I told this person, I said it in my last appointment.
Bill Gasiamis 1:26:23
Yeah. And it’s just what they’re doing is they’re double checking that they’ve got the right person in front of them that they are talking about the right and that’s all we need to do is okay. Okay, so what are you going to do about it? How you can help me? Why are we doing this? What’s the purpose of that? Why aren’t we doing this? Why aren’t we doing that? And you can do it nicely, you can have a lovely conversation with one of your medical professionals. If they don’t like it, that answering questions, well, then they’re the wrong person, and then you should fire them and you should move on and get somebody to help.
Jenn Williams 1:26:53
And I had one neurologist that my first appointment with her she was the other neurologist had left the practice and they had someone new. And during my appointment, she kept looking at her smartwatch. And she was like giggling, and so she was clearly reading messages on her smartwatch. And I got home, I was so angry. And my husband was like, try talking to her about it. Just try talking to her about it.
Jenn Williams 1:27:22
She’s new to the area, she’s the only one in the area. So see if you can work it out with her. And my next appointment, I said, I need to tell you that at my last appointment, I did not feel like you were as invested in my care as I am. And I really need us to be on the same page. And she sat right up and I’m like, oh, oh, I’m so sorry. I didn’t mean to do that.
Jenn Williams 1:27:45
Blah, blah, blah. And we had a great relationship until she moved again, gone through a lot of neurologists, but even just saying that, in my previous life, I would not have said that. I wouldn’t have ever said something like that. But I did. And it worked out and we got on the same page. And we took steps for my recovery. And it felt very collaborative. So even just saying something like that made a huge difference.
Thalamic Stroke Recovery, Grief, And Resilience
Bill Gasiamis 1:28:16
Excellent. What would you like to say to some of the stroke survivors that are listening, that are just on their journey or a few years down the track? Things are a little bit challenging for them? What do you want to say to them?
Jenn Williams 1:28:33
Recovery is not a sprint. It’s a marathon. It is not three months, it is not a year, it is not two years. It is a life altering journey. And I will tell you, I probably spent the first three years of my recovery and grief. And once I got through all of that I was able to give back. I was able to start helping people and speak at support groups and do self advocacy work. And there’s a lot of really beautiful things that can happen on the other side of that grief. You just have to hang in there.
Bill Gasiamis 1:29:13
Thank you so much for joining me on the podcast. I really appreciate it.
Jenn Williams 1:29:20
Thank you. It was really nice to be here. I really appreciate it. I love talking about brain injury.
Bill Gasiamis 1:29:26
Me too. You wouldn’t have guessed from the 310 episodes. But yeah, I don’t mind that either. Thanks so much, Jen.
Jenn Williams 1:29:40
Thanks, Bill.
Bill Gasiamis 1:29:42
Thanks for joining us on today’s episode. If you are interested in a copy of my book about stroke recovery. You can grab a copy on Amazon by visiting on Amazon or by visiting recoveryafterstroke.com/book to learn more more about my guests including links to their social media and to download a full transcript. Head over to recoveryaftershow.com/episodes.
The post Thalamic Stroke: Symptoms, Treatment, and Recovery appeared first on Recovery After Stroke.
301 قسمت
همه قسمت ها
×به Player FM خوش آمدید!
Player FM در سراسر وب را برای یافتن پادکست های با کیفیت اسکن می کند تا همین الان لذت ببرید. این بهترین برنامه ی پادکست است که در اندروید، آیفون و وب کار می کند. ثبت نام کنید تا اشتراک های شما در بین دستگاه های مختلف همگام سازی شود.